Understanding Anti-Androgens for Advanced Prostate Cancer
Explore how anti-androgen therapies play a vital role in managing advanced prostate cancer, including treatment options, benefits, and potential side effects.
Prostate cancer is a pressing health concern for men worldwide, with advanced stages often requiring more complex treatment strategies. Among the primary approaches to managing advanced and metastatic prostate cancer is hormone therapy—specifically, the use of anti-androgens to halt or slow cancer growth. This article offers a comprehensive look at anti-androgen therapy: how it works, types of available drugs, possible side effects, and what patients can expect during treatment.
What Are Anti-Androgens?
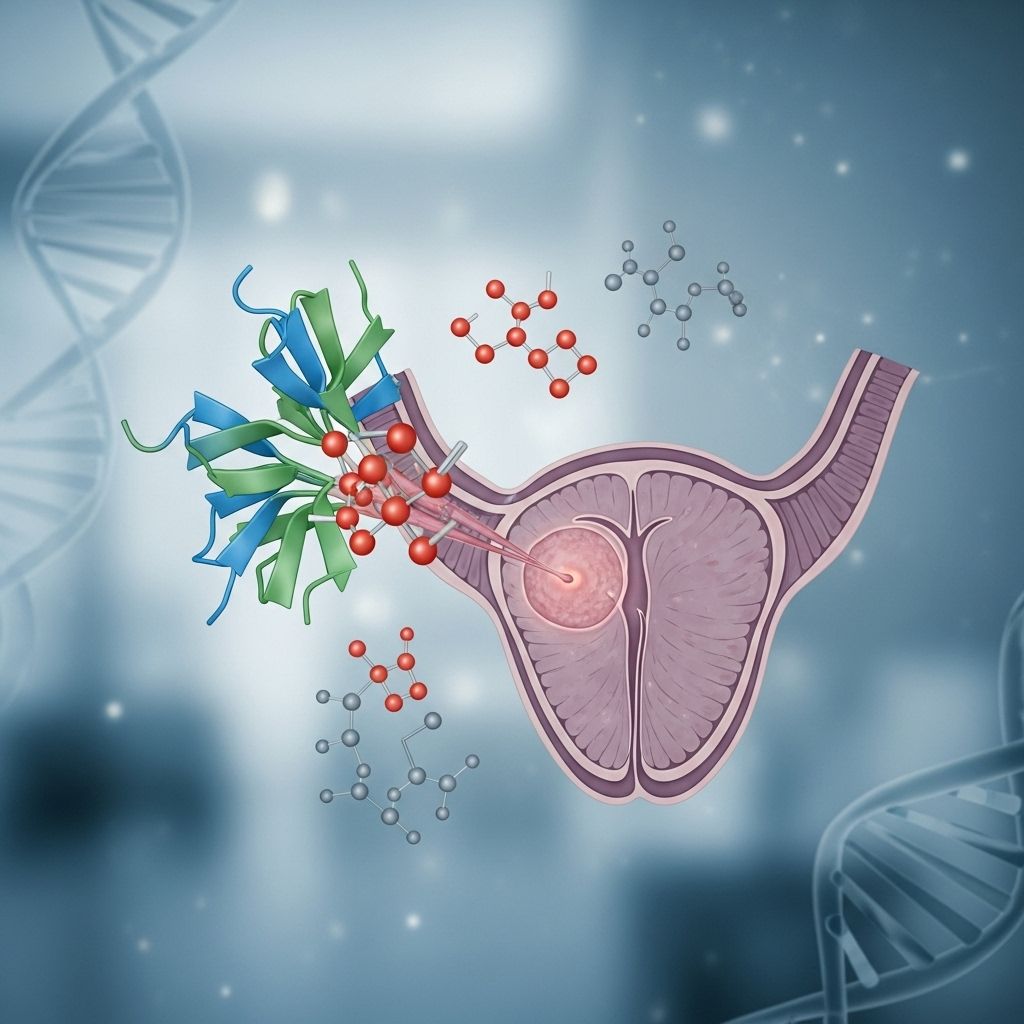
Anti-androgens, also known as androgen receptor antagonists, are drugs designed to block the action of androgens—mainly the male hormone testosterone—on prostate cancer cells. Testosterone and other androgens fuel the growth of most prostate cancers by binding to androgen receptors present in these cells. By preventing this hormonal connection, anti-androgens help limit cancer cell growth and symptoms.
- Androgens: Hormones that stimulate the development and maintenance of male characteristics, with testosterone being the most significant.
- Androgen Receptors: Proteins on prostate cells that bind to androgens, enabling their effects on cell growth.
- Anti-Androgens: Medications that block androgens from binding to their receptors.
Role of Androgens in Prostate Cancer
The prostate gland is highly sensitive to androgen stimulation. Androgens not only contribute to normal prostate function but also play a major role in the proliferation of cancer cells.
- Prostate cancer cells depend on androgens to grow and survive.
- When androgen levels are lowered or their effect is blocked, the progression of prostate cancer can be slowed or stopped for a time.
How Do Anti-Androgens Work?
Anti-androgens function by binding to androgen receptors on prostate cancer cells. This binding blocks the cells from receiving growth signals provided by circulating androgens. As a result:
- Tumor growth is inhibited or slowed.
- Symptoms such as pain or urinary complications can be reduced or managed.
Most anti-androgen therapies do not reduce androgen levels in the body but rather block their action at the cellular level. They are often administered in conjunction with other hormone-suppressing therapies to optimize treatment outcomes.
Types of Anti-Androgens
Anti-androgens can be categorized into first-generation and second-generation drugs, each with distinct mechanisms and clinical applications.
First-Generation Anti-Androgens
- Flutamide (Eulexin): One of the earliest anti-androgens used, administered orally.
- Bicalutamide (Casodex): More widely used due to a better side effect profile; taken by mouth.
- Nilutamide (Nilandron): Also taken orally, sometimes used when others are ineffective.
These medications are typically combined with therapies that lower androgen levels, such as surgical castration (orchiectomy) or luteinizing hormone-releasing hormone (LHRH) agonists and antagonists. This combination is referred to as combined androgen blockade (CAB) or complete androgen blockade.
Second-Generation Anti-Androgens
Second-generation anti-androgens have been developed to provide improved potency and broader efficacy, particularly in cases where cancer has become resistant to earlier treatments.
- Enzalutamide (Xtandi): Approved for metastatic castration-resistant and castration-sensitive prostate cancer; blocks androgen receptor signaling more effectively.
- Apalutamide (Erleada): Used for non-metastatic castration-resistant and metastatic castration-sensitive prostate cancer.
- Darolutamide (Nubeqa): Offers similar benefits with potentially fewer central nervous system side effects.
When Are Anti-Androgens Used?
Anti-androgens are integrated into prostate cancer treatment in several scenarios, including:
- As first-line therapy for advanced or metastatic prostate cancer, usually in combination with other hormone-lowering interventions.
- As part of combined androgen blockade for patients whose cancer remains sensitive to hormonal manipulation.
- For patients whose cancer has become castration-resistant—meaning it continues to grow despite low testosterone levels.
- Sometimes as a secondary hormonal manipulation when resistance to primary therapy develops.
Combining Anti-Androgens with Other Treatments
Optimal prostate cancer care often involves combining anti-androgens with other treatments, such as:
- Androgen deprivation therapy (ADT): The mainstay of hormonal treatment, which includes surgical or medical castration via LHRH agonists or antagonists.
- Androgen synthesis inhibitors: Medications like abiraterone acetate (Zytiga) that block androgen production within the adrenal glands and tumor cells.
- Chemotherapy: Agents like docetaxel for more advanced, treatment-resistant cases.
- Radiopharmaceuticals: For patients with bone metastases, drugs such as radium-223 dichloride may be used.
Hormone Therapy and Castration-Resistant Prostate Cancer
Some prostate cancers eventually become resistant to treatments that reduce androgen levels or block androgen receptors—a condition termed castration-resistant prostate cancer (CRPC). Management strategies for CRPC include:
- Continued ADT, as the cancer may still rely on minimal androgen activity.
- Switching to second-generation anti-androgens or androgen synthesis inhibitors.
- Addition of immunotherapy, such as sipuleucel-T, or innovative treatments like PARP inhibitors for suitable patients.
- Chemotherapy and targeted radiopharmaceuticals for advanced, symptomatic cases.
Common Side Effects of Anti-Androgens
While anti-androgens are generally well-tolerated, they may cause a range of side effects due to suppressed androgen signaling. Most side effects are manageable but can impact quality of life. Common side effects include:
- Gynecomastia: Enlargement or tenderness of breast tissue.
- Hot flashes: Sudden feelings of warmth, sweating.
- Decreased libido and erectile dysfunction.
- Gastrointestinal issues: Nausea, diarrhea, liver function abnormalities (mainly with flutamide).
- Fatigue.
- Potential changes in mood or cognition (especially with some second-generation agents).
Each individual responds differently, and side effect severity can depend on the chosen medication and overall health.
Monitoring and Managing Treatment
Effective management of advanced prostate cancer requires regular monitoring to assess response and detect possible resistance or adverse effects. Key aspects include:
- Regular PSA measurements: Prostate-specific antigen (PSA) blood tests to track cancer activity.
- Imaging: CT scans, bone scans, or MRI to detect recurrence or progression to other organs.
- Routine lab tests: Liver and kidney function, hormone levels, and blood counts depending on treatment.
Communication between patient and provider is crucial to adapt therapy as needed and optimize quality of life.
Weighing the Benefits and Risks
The decision to start or continue anti-androgen therapy involves balancing potential benefits against risks and side effects. Considerations include:
- Improved cancer control: Suppression of tumor growth, slowing disease progression, and symptom relief.
- Side effects: Potential impact on sexual function, bone health, mood, and metabolism.
- Impact on longevity and quality of life.
- Individual factors: Age, other medical conditions, previous treatments, and patient preferences.
Current and Emerging Strategies
While many patients respond well to initial anti-androgen strategies, resistance often develops over time due to changes in androgen receptor function or additional cancer cell mutations. Newer treatment approaches aim to overcome such resistance, including:
- Switching to second-generation or newer agents.
- Adding androgen synthesis inhibitors such as abiraterone (often combined with prednisone), which target androgen production throughout the body, including in the adrenal glands and the tumor itself.
- Combination therapies that attack cancer via multiple mechanisms, including immune modulation and genetic targeting (e.g. PARP inhibitors).
- Anti-androgen withdrawal: In some cases, simply stopping anti-androgen drugs leads to temporary improvement, likely due to complex changes in cancer cell response. This is sometimes tried before moving to next-line therapies.
Questions to Ask Your Healthcare Team
Patients are encouraged to take an active role in their treatment. Some questions for discussion include:
- Which anti-androgen options are most appropriate for my specific condition?
- What side effects should I watch for, and how can they be managed?
- Are there lifestyle changes or supportive treatments that can improve my outlook or well-being?
- How will we monitor my response and adjust my treatment over time?
Comparative Table: First vs. Second-Generation Anti-Androgens
| Drug Type | Examples | Typical Use | Key Benefits | Common Drawbacks |
|---|---|---|---|---|
| First-Generation | Flutamide, Bicalutamide, Nilutamide | Initial or adjunct therapy; often with ADT | Effective, widely available | GI side effects, occasional liver toxicity, resistance develops |
| Second-Generation | Enzalutamide, Apalutamide, Darolutamide | Castration-resistant prostate cancer, advanced settings | Higher efficacy, works in resistant cancers | Fatigue, risk of seizures (rare), higher cost |
Frequently Asked Questions (FAQ)
What is the purpose of anti-androgen therapy in prostate cancer?
Anti-androgen therapy is used to directly block the action of androgens on prostate cancer cells, which helps slow or prevent the growth of tumors.
Are anti-androgens used alone or with other treatments?
Although they can be used alone, anti-androgens are often prescribed with other hormone therapies, such as androgen deprivation therapy, for optimal control of advanced prostate cancer.
What are the most common side effects of anti-androgens?
Patients may experience hot flashes, breast tenderness, reduced libido, fatigue, or gastrointestinal symptoms, among others.
What happens if my cancer becomes resistant to anti-androgens?
If resistance occurs, your provider will likely propose alternative strategies such as newer generation drugs, androgen synthesis inhibitors, chemotherapy, or targeted therapies.
How will I know if anti-androgen therapy is working?
Your healthcare team will monitor your PSA levels, conduct regular imaging, and assess your symptoms to determine treatment effectiveness.
Summary
Anti-androgen therapy remains a cornerstone in the management of advanced prostate cancer. While the choice of drug and duration of use may vary based on individual needs and how the cancer responds to treatment, ongoing research and new drug development continue to expand options and improve outcomes. Open dialogue with healthcare providers ensures that therapy is tailored, side effects are managed, and quality of life is prioritized at every stage.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3172154/
- https://www.cancer.gov/types/prostate/prostate-hormone-therapy-fact-sheet
- https://www.cancer.org/cancer/types/prostate-cancer/treating/hormone-therapy.html
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6976485/
- https://zerocancer.org/stages-and-treatment/systemic-therapies/hormone-therapy
- https://www.mayoclinic.org/tests-procedures/hormone-therapy-for-prostate-cancer/about/pac-20384737
- https://www.cancercouncil.com.au/prostate-cancer/management-treatment/androgen-deprivation-therapy/
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/prostate-cancer-androgen-deprivation-therapy
Read full bio of medha deb












