Angioplasty and Stent Placement for the Heart: Procedure, Recovery, and Risks
Discover how angioplasty and stent placement restore heart blood flow, what to expect from the procedure, and crucial aftercare insights.
Angioplasty and Stent Placement for the Heart
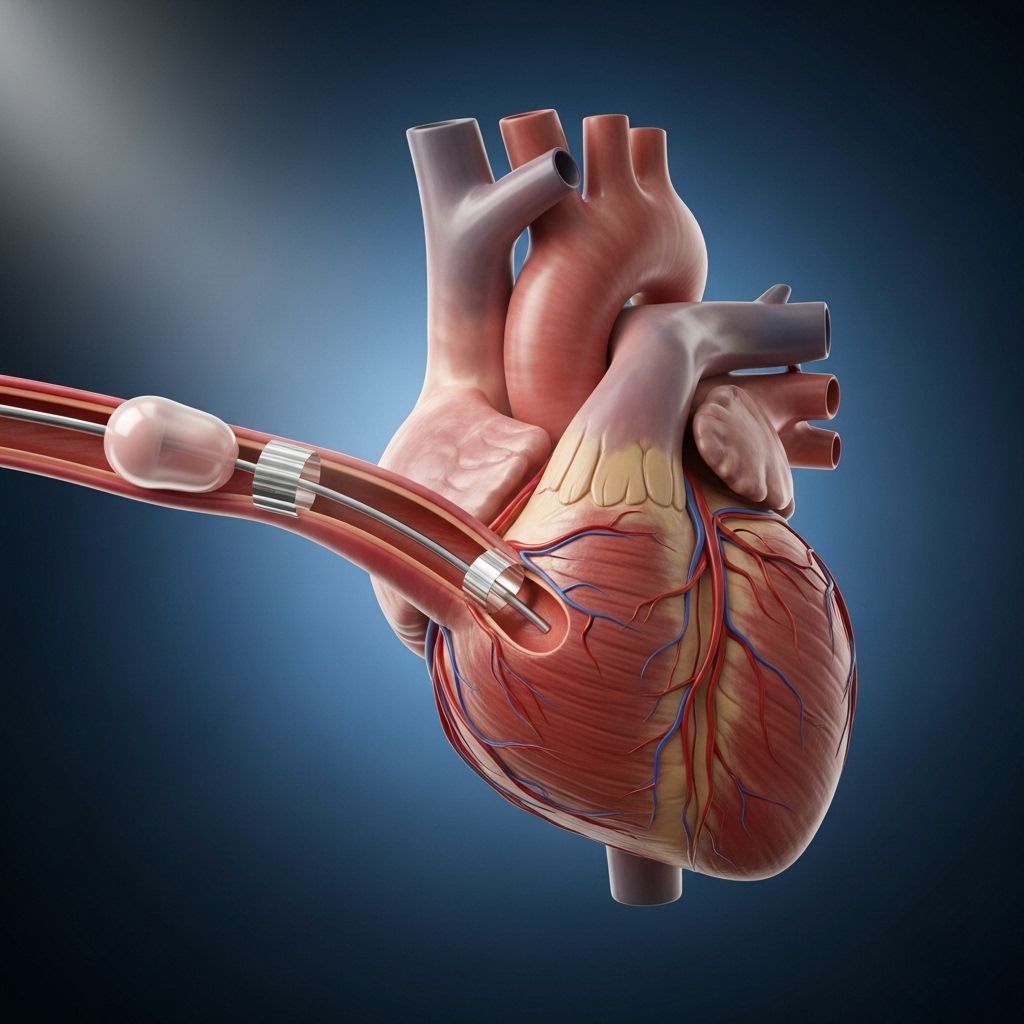
Angioplasty and stent placement are vital medical procedures used to treat coronary artery disease by restoring blood flow to the heart muscle. These minimally invasive interventions have transformed the management of heart blockages, offering rapid symptom relief and reducing the risk of heart attacks for millions of patients worldwide.
What Are Coronary Arteries and Why Do They Become Blocked?
The coronary arteries supply oxygen-rich blood to the heart muscle. Over time, these arteries can narrow or become blocked by fatty deposits (plaques), leading to reduced blood flow. This condition is known as coronary artery disease (CAD) and can result in chest pain (angina), heart attacks, and other serious complications.
- Plaque buildup is typically caused by atherosclerosis—a process involving cholesterol, fat, and other substances accumulating along artery walls.
- Symptoms of blocked arteries include chest discomfort, shortness of breath, fatigue, and in severe cases, heart attack.
What Is Angioplasty?
Angioplasty (also known as percutaneous coronary intervention or PCI) is a procedure designed to open narrowed or blocked coronary arteries. It involves inserting a small, flexible tube called a catheter into an artery, often in the wrist or groin, and guiding it to the heart. A balloon at the catheter tip is then inflated to compress plaque against the artery wall, improving blood flow.
Main Steps of Angioplasty Procedure
- The patient receives sedation and blood-thinning medications via an intravenous (IV) line.
- A cardiologist inserts the catheter into an access artery (wrist, arm, or groin).
- Using live X-ray imaging (fluoroscopy), the catheter is advanced up to the heart.
- Contrast dye is injected to visualize the arteries and locate blockages.
- A guide wire is threaded past the blockage.
- A balloon catheter is positioned at the narrowed section and inflated to widen the artery.
How Does Stent Placement Work?
Stent placement typically occurs during angioplasty to help keep the artery open long-term.
- A stent is a small, expandable metal mesh tube.
- The stent is mounted on a balloon catheter and delivered to the blockage.
- When the balloon inflates, the stent expands and presses against the artery wall.
- The balloon is then deflated and removed, leaving the stent in place.
- Most modern stents are drug-eluting—they release medication to help prevent future narrowing (restenosis).
Why Is Angioplasty and Stent Placement Needed?
This procedure is recommended for people with significant narrowing of their coronary arteries causing symptoms (e.g., chest pain, shortness of breath) or acute events like heart attacks. It can quickly restore blood flow, alleviate symptoms, and prevent damage to the heart muscle.
| Indication | Typical Goals |
|---|---|
| Angina (chest pain) | Relieve symptoms, improve quality of life |
| Acute heart attack (MI) | Restore blood flow to prevent heart muscle damage |
| High-risk blockages | Reduce risk of future cardiac events, provide long-term vessel patency |
Types of Stents Used in Coronary Procedures
- Bare-metal stents: Provide mechanical support but do not release medication. Risk of restenosis is higher.
- Drug-eluting stents: Coated with medication that helps reduce recurrence of artery narrowing. Now considered standard due to superior outcomes.
How to Prepare for Angioplasty and Stent Placement
Patients typically undergo a series of evaluations before the procedure:
- Blood tests to assess kidney function, clotting status, and overall health.
- An electrocardiogram (EKG) and possibly imaging (echocardiography, stress testing).
- Certain medications (e.g., blood thinners, anti-platelet drugs) may be started beforehand.
- Do not eat or drink for a set period before the procedure (usually 6–8 hours).
Inform your medical team about allergies, especially to contrast dye or medications, and other medical conditions (kidney disease, bleeding disorders).
What Happens During the Procedure?
- The patient lies on a procedure table, attached to monitors for heart rate, blood pressure, and oxygen levels.
- IV sedation is administered via a vein in the hand or arm.
- The insertion area (wrist, arm, or groin) is cleaned, sterilized, and numbed with a local anesthetic.
- A small incision is made to access the artery; a sheath is inserted as an entry port for catheters.
- Using imaging guidance, the catheter reaches the heart’s arteries.
- Contrast dye is injected, allowing the physician to locate blockages with live X-rays (angiogram).
- A guide wire and balloon catheter are positioned at the block and inflated to open the artery.
- If needed, the stent is deployed.
- If multiple blockages exist, the process is repeated as required.
Recovery After Angioplasty and Stent Placement
After the procedure, patients are closely monitored for several hours. Most recover in a designated cardiac care area of the hospital, and observation continues to ensure stable heart function and to check for complications.
- Vital signs (heart rate, blood pressure) are monitored.
- The access site (wrist/groin) is observed for bleeding, swelling, or infection.
- Most patients remain in hospital overnight.
- Early mobilization is possible in many cases, especially if the wrist approach is used.
Home Care After Discharge
- Follow instructions regarding wound care and medication regimen: anti-platelet drugs (aspirin, clopidogrel) are often prescribed to prevent stent clotting.
- Avoid strenuous activity and heavy lifting for several days to a week.
- Watch for signs of infection: fever, redness, swelling, or unusual pain at the incision site.
- Report chest pain, shortness of breath, or irregular heartbeat to your doctor immediately.
- Attend scheduled follow-up appointments to monitor recovery and adjust medications as needed.
Benefits of Angioplasty and Stenting
- Relieves symptoms like chest pain or shortness of breath quickly.
- Restores blood flow to the heart muscle, reducing risk of heart damage.
- Minimally invasive: shorter recovery time compared to open-heart surgery.
- Reduces future cardiovascular events in patients with significant blockages.
Potential Risks and Complications
While angioplasty and stenting are generally safe, they do carry some risks. Your healthcare team will discuss these with you to ensure informed consent.
- Bleeding or bruising at the catheter insertion site.
- Infection.
- Blood vessel damage.
- Allergic reaction to contrast dye.
- Re-narrowing (restenosis) of treated artery, less common with drug-eluting stents.
- Blood clot formation within or around the stent (stent thrombosis)—necessitates anti-platelet medication adherence.
- Heart attack, stroke, or (rarely) death.
Comparing Angioplasty and Stent Placement to Other Treatments
| Treatment | Advantages | Disadvantages |
|---|---|---|
| Angioplasty & Stenting | Minimally invasive, rapid recovery, effective symptom relief | Possible recurrence of blockage, need for medication compliance |
| Coronary Artery Bypass Surgery (CABG) | Bypasses multiple blockages, durable long-term results | Major surgery, longer recovery, higher initial risk |
| Medication Alone | Non-invasive | May not suffice for severe blockages, ongoing symptoms possible |
Frequently Asked Questions (FAQs)
Q1: Will I be awake during angioplasty?
Most patients are awake but given sedating medication to help them relax. General anesthesia is rarely needed unless the patient’s condition requires it.
Q2: How long does the procedure take?
The procedure generally lasts from 30 minutes to 2 hours, depending on the complexity and number of blockages.
Q3: How soon can I resume normal activities?
Most patients can walk within hours and return to everyday activities in a few days. Vigorous exercise or heavy lifting should wait at least one week, based on your doctor’s advice.
Q4: Is angioplasty a permanent cure for heart disease?
No. While it effectively opens blocked arteries, lifestyle changes and medications are needed to control heart disease long-term.
Q5: What are signs of complications after the procedure?
- Bleeding or swelling at the catheter site
- Fever, chills, or severe pain
- Recurrence of chest pain or shortness of breath
Q6: What happens if a stent develops a blood clot?
This is a potentially serious complication; anti-platelet medicines are vital for several months after stent placement to help prevent this event.
Q7: What lifestyle habits support recovery and heart health after angioplasty?
- Maintain a heart-healthy diet low in saturated fat, cholesterol, and sodium.
- Exercise regularly, as advised by your healthcare team.
- Quit smoking and limit alcohol use.
- Control blood pressure, cholesterol, and diabetes as directed.
Key Takeaways
- Angioplasty and stent placement are essential interventions for coronary artery disease, offering rapid relief of symptoms and improved heart function.
- The procedures involve opening blocked arteries and supporting them with a stent, often releasing medication to minimize recurrence.
- Risks include bleeding, re-narrowing, infection, and rare major complications— but overall, the benefits far outweigh these risks for suitable candidates.
- Recovery is usually rapid, but ongoing management through medications and lifestyle changes is crucial for long-term heart health.
More Patient Questions
How do I know if I am a candidate for angioplasty?
Your physician will assess your symptoms, medical history, test results, and severity of artery narrowing to determine if angioplasty and stenting are safe and appropriate for you.
Can stents set off airport metal detectors?
No—in most cases, modern stents do not trigger security alarms or metal detectors. You may request a card from your hospital documenting the presence of a stent.
What is the success rate of the procedure?
The vast majority of angioplasties and stent placements have high success rates with significant symptom improvement and reduced cardiac risk.
Do I need to take medicine after stent placement?
Yes, anti-platelet drugs are necessary to prevent stent clotting and reduce the risk of cardiovascular events. Your regimen will be personalized by your medical team.
Will I need repeat procedures?
While restenosis rates have dropped due to drug-eluting stents, some patients require follow-up angioplasties if new blockages occur or symptoms return.
References
- https://medlineplus.gov/ency/article/007473.htm
- https://www.mayoclinic.org/tests-procedures/coronary-angioplasty/about/pac-20384761
- https://www.youtube.com/watch?v=foLffy8FGjI
- https://www.radiologyinfo.org/en/info/angioplasty
- https://www.mountsinai.org/health-library/discharge-instructions/angioplasty-and-stent-heart-discharge
- https://www.nhs.uk/tests-and-treatments/coronary-angioplasty/
- https://my.clevelandclinic.org/health/treatments/22060-angioplasty
- https://www.nhlbi.nih.gov/health/stents/during
- https://www.heartandstroke.ca/heart-disease/treatments/surgery-and-other-procedures/percutaneous-coronary-intervention
Read full bio of Sneha Tete












