Angioplasty After a Heart Attack: Procedure, Benefits, and Risks
Understanding the angioplasty process after a heart attack, including its procedure, benefits, risks, and what to expect during recovery.
Angioplasty After a Heart Attack: Comprehensive Overview
Angioplasty is a crucial medical intervention performed to restore blood flow in blocked or narrowed coronary arteries, especially after a heart attack. As one of the leading emergency treatments, angioplasty can mean the difference between swift recovery and serious complications. This article details how angioplasty works, what to expect, its benefits and risks, and answers to common questions about the procedure.
What is Angioplasty?
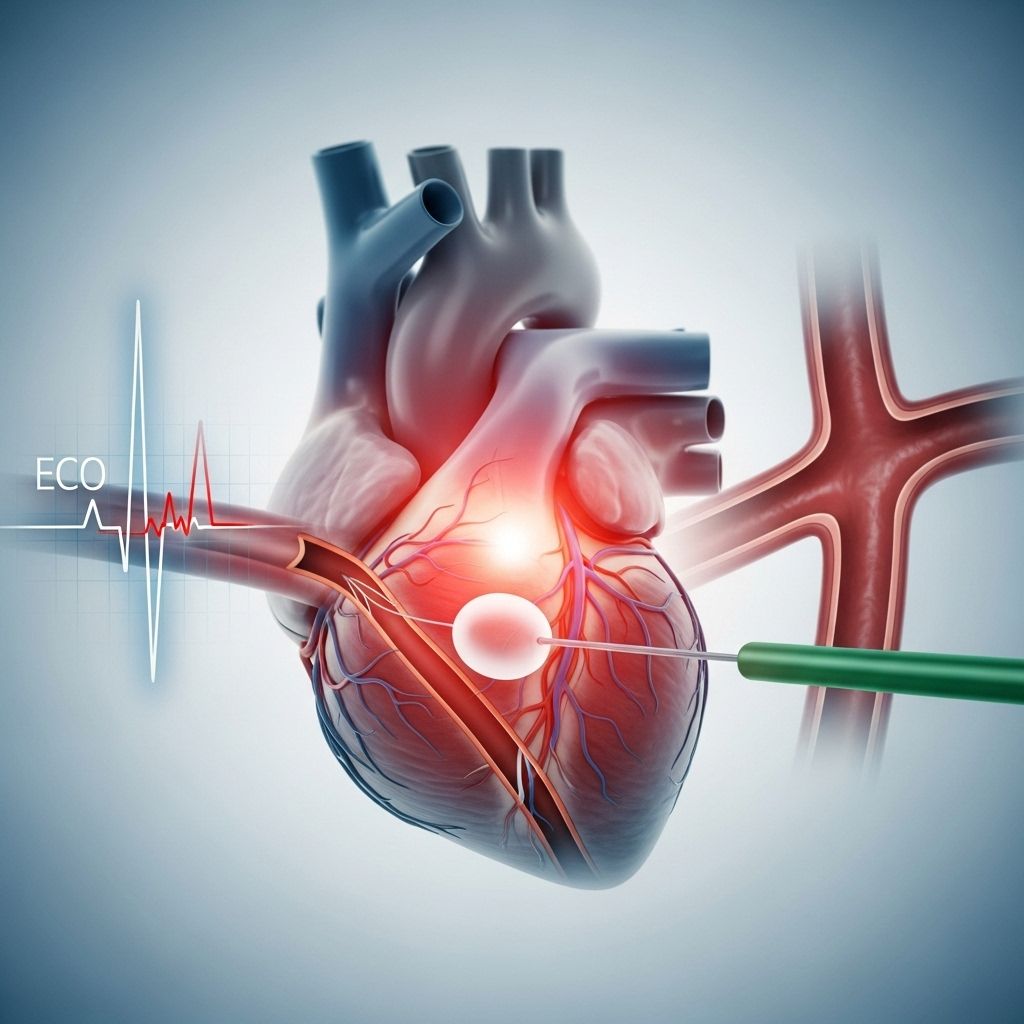
Angioplasty, also known as percutaneous transluminal coronary angioplasty (PTCA) or percutaneous coronary intervention (PCI), is a minimally invasive procedure designed to open up blocked or narrowed arteries that supply blood to the heart muscle. These coronary arteries can become clogged due to the build-up of fatty deposits known as plaque. When plaque accumulation leads to a heart attack, an angioplasty is often performed as an emergency measure to restore blood flow quickly and reduce heart damage.
In many cases, a stent—a tiny mesh tube—is inserted during angioplasty to help keep the artery open and maintain improved blood flow long-term.
Why is Angioplasty Needed After a Heart Attack?
During a heart attack, prompt restoration of blood flow is essential to preserve heart muscle and function. Angioplasty is often the first choice treatment because:
- It rapidly reopens the blocked artery.
- Reduces the risk of extensive heart muscle damage.
- Improves survival rates compared to medication-only approaches.
- Minimizes the risk of heart failure and other complications post-attack.
Doctors aim to perform angioplasty within the first 90 minutes of a patient’s arrival at the hospital and generally no later than 12 hours after symptom onset.
How is Angioplasty Performed?
The angioplasty procedure is typically done under local anesthesia. Here is a step-by-step outline of what happens:
- Preparation: The patient is given a mild sedative and a local anesthetic at the site where the catheter will be inserted—often the groin or arm. Monitoring equipment tracks the patient’s heart rhythm and vital signs.
- Catheter Insertion: A small incision is made, and a thin tube called a catheter is inserted into an artery. With the help of real-time X-ray imaging and a special contrast dye, the cardiologist advances the catheter through blood vessels toward the heart and into the affected coronary artery.
- Balloon Inflation: Once in place, a tiny balloon at the tip of the catheter is gently inflated. This balloon presses the plaque against the artery wall, opening the vessel and restoring blood flow.
- Stent Placement: In most cases, a stent (a small, expandable metal mesh tube) is placed at the site. The stent remains in place after the balloon and catheter are removed. Some stents are coated with medication to reduce the risk of the artery narrowing again (drug-eluting stents).
- Completion: The balloon is deflated, and the catheter is removed. Occasionally, pressure or a closure device is applied at the insertion site to stop bleeding and aid healing.
The entire procedure typically takes from 30 minutes up to several hours, depending on the complexity of the blockage and number of arteries involved.
Recovery After Angioplasty
Recovery usually involves a short hospital stay—often 1-2 days if there are no complications. Patients are monitored to ensure there are no immediate post-procedure issues such as bleeding, arrhythmias, or chest pain.
Benefits of Angioplasty After a Heart Attack
Angioplasty offers several significant advantages, especially when performed quickly after a heart attack:
- Fast Restoration of Blood Flow: Minimizes heart muscle damage and limits the severity of the heart attack.
- Reduced Risk of Complications: Lowers the risk of developing heart failure or life-threatening arrhythmias.
- Increased Survival Rate: Studies show improved survival rates for patients receiving timely angioplasty.
- Improved Symptom Relief: Rapidly alleviates chest pain (angina) and shortness of breath, both during a heart attack and in chronic coronary artery disease.
- Avoidance of More Invasive Surgery: May prevent the need for open-heart surgery such as coronary artery bypass grafting (CABG), which involves longer hospital stays and a lengthier recovery.
- Lower Recurrent Heart Attack Risk: Sustained blood flow reduces the chances of a second heart attack compared to medication-only management.
Risks and Possible Complications of Angioplasty
As with any invasive procedure, angioplasty carries some risks, though most are low and manageable. Potential complications include:
- Allergic reactions to anesthesia, contrast dye, or materials used in the stent.
- Bleeding or bruising at the catheter insertion site.
- Blood clots or scar tissue developing within the stent (which may require additional intervention).
- Irregular heartbeat (arrhythmia).
- Damage to blood vessels, heart valves, or coronary arteries.
- Infection at the incision or inside blood vessels.
- Kidney injury from contrast dye, particularly in people with preexisting kidney problems.
- Stroke (rare occurrence).
- Restenosis: Artery may become narrow again, especially if a stent was not used or if lifestyle and medication guidelines are not followed.
The risks are somewhat higher in emergency angioplasty immediately after a heart attack due to the urgency and the patient’s unstable condition. However, the potential benefits greatly outweigh these risks in most cases.
Who is a Candidate for Angioplasty?
Angioplasty is recommended for:
- Most patients experiencing an acute heart attack (especially ST-elevation myocardial infarction or STEMI).
- People with severe angina not relieved by medications.
- Certain cases of chronic coronary artery disease, where blockages are limiting quality of life or heart function.
Some patients may not be suitable for angioplasty, such as those with very widespread (diffuse) disease, left main coronary artery blockage, or multiple vessel disease combined with diabetes. In these cases, coronary artery bypass surgery may be recommended.
What Happens After Angioplasty?
Post-procedure care focuses on ensuring proper healing, monitoring for complications, and preventing future arterial blockages. Common aspects of recovery and follow-up care include:
- Observation: Patients are monitored for a few hours up to two days for complications.
- Medication: Blood-thinning medications (antiplatelets) like aspirin and clopidogrel are often prescribed to prevent blood clots in the stent. Other medications may include statins to lower cholesterol, beta-blockers, or ACE inhibitors.
- Incision Care: Instructions on keeping the insertion site clean and monitoring for signs of infection.
- Lifestyle Modifications: Diet, exercise, and quitting smoking are essential for long-term heart health and preventing re-narrowing (restenosis).
- Cardiac Rehabilitation: Structured exercise and education programs help with a safe recovery and improve long-term outcomes.
Most people return to normal activities within a week, but heavy lifting and strenuous exercise should be avoided for several days, as per doctor guidance.
Outlook After Angioplasty
The overall outlook after angioplasty is positive for most people. When performed promptly, it significantly enhances survival, limits heart muscle damage, and improves quality of life. However, it’s important to remember that angioplasty is not a cure for heart disease. Lifelong adherence to medication, heart-healthy lifestyle changes, and regular medical follow-up are essential to maintain artery health and prevent recurrence.
Angioplasty vs. Other Treatments
| Criteria | Angioplasty/PCI | Coronary Artery Bypass Grafting (CABG) | Medication/ Thrombolysis |
|---|---|---|---|
| Speed | Very rapid (minutes to hours) | Slower (requires open-heart surgery, days of preparation) | Immediate (if administered early) |
| Hospital Stay | Short (1-2 days) | Longer (5-7 days or more) | Variable (can be outpatient) |
| Recovery Time | Faster (days to one week) | Slower (weeks to months) | Rapid if no complications |
| Suitability | Best for single/multiple blockages in suitable arteries | Best for left main/multiple complex artery blockages, diabetes | Best if PCI not available immediately, some mild cases |
| Long-Term Results | Excellent when combined with lifestyle and medication | Excellent for complex disease | Higher recurrence risk |
Frequently Asked Questions (FAQs)
What symptoms suggest I might need an angioplasty?
If you have chest pain or discomfort, shortness of breath, pain radiating to your jaw or arm, or unexplained sweating—especially during activity or rest—consult a doctor immediately. These could be signs of a heart attack or unstable angina that might require angioplasty.
How long does the angioplasty procedure take?
A standard coronary angioplasty procedure may last from 30 minutes up to several hours, depending on the number and location of blockages.
Will I need a stent during angioplasty?
In most cases, a stent is recommended after angioplasty to help keep the artery open and reduce the chance of re-narrowing (restenosis). Your doctor will determine the best approach for you.
Is recovery from angioplasty painful?
Most patients experience minimal pain. Some report mild soreness, bruising, or discomfort at the catheter insertion site, which typically resolves within a few days.
How do I reduce the risk of my arteries narrowing again?
Maintain a heart-healthy diet, follow your doctor’s medication plan (especially blood thinners), exercise regularly, avoid smoking, and keep blood pressure, blood sugar, and cholesterol under control.
Are there alternatives to angioplasty?
Alternatives include medications to dissolve clots (thrombolysis), open-heart surgery (bypass), and long-term management with medications and lifestyle changes. The most suitable option depends on individual health conditions and artery blockage location.
Final Thoughts
Angioplasty is a life-saving procedure for many people experiencing heart attacks or severe coronary artery disease. Its benefits are most pronounced when performed quickly and followed by lifestyle modification and vigilant post-procedure care. Always consult your healthcare provider for personalized medical advice and never ignore warning symptoms of heart disease.
References
- https://www.healthline.com/health/heart-attack/angioplasty
- https://www.healthline.com/health/angioplasty-and-stent-placement-heart
- https://medlineplus.gov/ency/article/000195.htm
- https://www.mayoclinic.org/diseases-conditions/heart-attack/diagnosis-treatment/drc-20373112
- https://www.medicalnewstoday.com/articles/237191
- https://info.health.nz/conditions-treatments/heart-health/heart-attack
- https://www.ebsco.com/research-starters/complementary-and-alternative-medicine/natural-treatments-heart-attacks
- https://www.echelon.health/heart-disease-in-women-symptoms-risk-factors/
- https://www.spirehealthcare.com/health-hub/specialties/heart-health/warning-signs-and-symptoms-of-a-heart-attack/
- https://www.britannica.com/science/heart-attack
Read full bio of Sneha Tete












