Angiogram vs Angioplasty: Key Differences, Purposes, and What to Expect
A comprehensive look at angiogram and angioplasty—understand their roles, procedures, risks, and impact on heart health.
If you’re experiencing chest pain or have been diagnosed with a heart problem, you may encounter the terms angiogram and angioplasty. While similar in name and often performed in the same clinical setting, these procedures differ greatly in their purpose, processes, and impact on your heart health. This article explores what sets them apart, when each is necessary, how they’re done, what recovery is like, and their implications for your future well-being.
Understanding Angiogram and Angioplasty
Both angiograms and angioplasties are minimally invasive procedures used in the investigation and treatment of blocked or narrowed arteries, especially those supplying blood to the heart (coronary arteries). Despite their similarities, they serve different functions within the field of cardiac care:
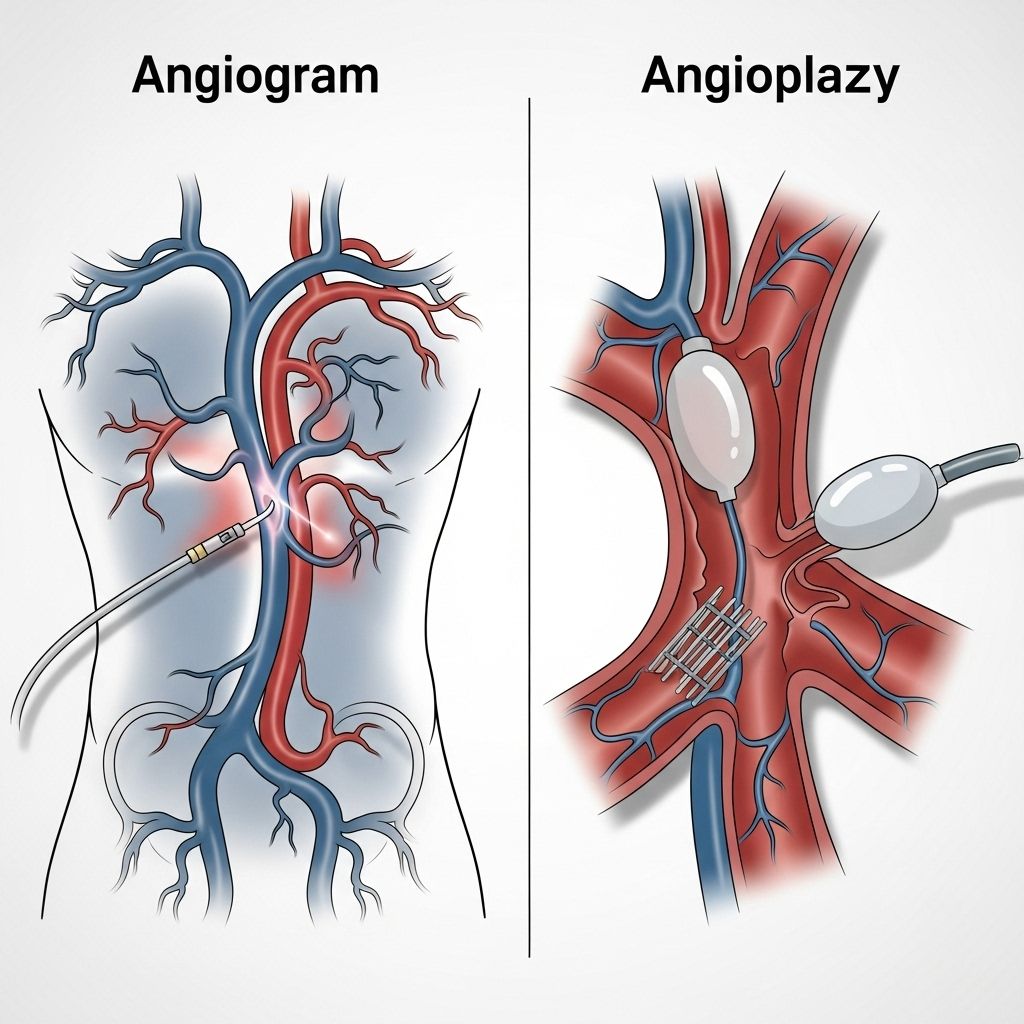
- Angiogram: a diagnostic imaging test that visualizes blood flow in your arteries using X-ray, CT, or MRI scans. It’s used to locate and assess blockages or narrowing within blood vessels.
- Angioplasty: a therapeutic intervention where a physician opens up blocked or narrowed arteries—most often with a balloon or a small mesh tube called a stent—to restore normal blood flow.
Both procedures are typically performed in a cardiac catheterization laboratory (“cath lab”) and are done on an outpatient basis, meaning you can usually return home the same day .
Are Angiogram and Angioplasty the Same?
No, and understanding the key differences can help you make better-informed decisions about your heart care. Here’s a concise breakdown:
| Aspect | Angiogram | Angioplasty |
|---|---|---|
| Purpose | Diagnosis—visualizes arteries to find blockages or narrowing | Treatment—opens blocked/narrowed arteries to restore blood flow |
| Procedure | Contrast dye injected, images captured via X-ray | Balloon (and often stent) inserted to widen artery |
| Performed When | Symptoms suggest possible blockages, or as follow-up to noninvasive tests | Blockage confirmed or diagnosed, requiring immediate intervention |
| Risk Level | Lower (mainly diagnostic) | Higher (involves artery intervention) |
| Outpatient? | Yes | Yes, but may require longer observation |
It’s common for an angiogram to lead directly to an angioplasty if blockages are found during the same session. The angiogram is essentially the roadmap—angioplasty is the repair work .
About the Procedures
Angiogram: Step-by-Step
- You’ll change into a hospital gown and lie on a procedure table in the cath lab. Your heart rate, blood pressure, and oxygen levels will be continuously monitored.
- An area on your wrist or groin is cleaned and numbed. A thin tube called a catheter is inserted through a blood vessel and carefully guided up toward your heart.
- A contrast dye is injected through the catheter to make your blood vessels visible on X-ray images.
- As the dye moves through your coronary arteries, real-time X-ray images are taken, revealing any blockages, narrowing, or irregularities.
- Depending on results, your team may recommend further intervention (like angioplasty) immediately or after more discussion.
Angioplasty: Step-by-Step
- The process begins much like an angiogram, with catheter insertion and imaging to locate the blockage.
- Once the blockage is found, a tiny balloon at the tip of the catheter is inflated at the site, compressing the plaque against the artery walls and widening the passage.
- Often, a stent (small mesh tube) is placed in the artery to keep it open. The balloon is then deflated and removed, but the stent remains in place.
- Final imaging ensures blood flow has been restored.
- You’ll remain under observation to monitor for any immediate complications.
Is One Always Performed Before the Other?
An angiogram is frequently done first, particularly when symptoms (such as chest pain, shortness of breath, abnormal stress test) indicate possible arterial narrowings or blockages. The angiogram identifies the problem areas. If significant blockages are found and criteria are met, an angioplasty might be performed right away, often in the same procedure session .
- In urgent or emergency cases (such as heart attacks), immediate angioplasty may be performed after a diagnostic angiogram.
- In elective or stable situations, your care team may schedule angioplasty for another day.
Heart Stents in Angioplasty
One of the most important advances in treating coronary blockages is the use of stents. These are tiny, expandable mesh tubes that support the inner wall of the artery after it’s been widened by balloon angioplasty.
- Drug-eluting stents (DES) release medication to help prevent the artery from becoming blocked again (restenosis).
- Bare-metal stents are less commonly used but may still be appropriate in certain cases.
- Stents significantly reduce the rate of artery re-narrowing compared to balloon angioplasty alone.
Placement of a stent means you’ll likely need to take antiplatelet medications (such as aspirin with clopidogrel) for an extended period to reduce the risk of blood clots forming in the stented artery .
Clearing Blockages and Restoring Blood Flow
Angioplasty (especially with stenting) actively treats blockages that could lead to chest pain, heart attack, or other cardiac events. Here’s how it helps:
- Improves blood flow to the heart muscle after a blockage.
- Reduces or eliminates symptoms like chest pain (angina) or shortness of breath.
- Can limit the amount of heart muscle damage during a heart attack.
- May serve as an alternative to more invasive surgery, such as coronary artery bypass grafting (CABG), in patients with less severe disease.
While angioplasty opens up narrowed arteries, it does not “cure” underlying coronary artery disease. Lifestyle changes and ongoing medical therapy are necessary to address the underlying process and reduce the risk of future blockages .
How Serious Are These Procedures?
Both angiogram and angioplasty are generally considered safe, minimally invasive procedures. However, the invasiveness, recovery time, and risks associated with angioplasty are somewhat higher compared to angiogram, mainly because angioplasty involves arterial intervention rather than diagnostic imaging alone.
- Angiogram risks: Allergic reaction to dye, minor bleeding or bruise at catheter site, rare risk of blood vessel injury or infection.
- Angioplasty risks: All the above, plus potential for re-narrowing (restenosis), blood clots, vessel or heart damage, heart attack, or need for emergency surgery (rare).
- Risk increases with age, presence of other diseases (like diabetes, kidney problems), or if the procedure is urgent or emergent.
Does Angioplasty or Angiogram Affect Life Expectancy?
Angiography alone is diagnostic and does not change life expectancy, but provides crucial information to help prevent heart attacks and guide future treatment choices. Angioplasty can improve survival and quality of life, particularly if:
- Performed promptly during a heart attack to restore blood flow and prevent further damage.
- Used in people with severe symptoms or those at high risk for cardiac events not controlled by medication or lifestyle changes.
However, since heart disease is a chronic condition, the biggest effect on long-term health comes from a combination of medical therapy, risk factor management (such as quitting smoking, controlling cholesterol and blood sugar), and ongoing lifestyle changes.
What to Expect Before, During, and After
Before the Procedure
- Follow instructions regarding when to stop eating and which medications to take.
- Inform your medical team of allergies, especially to contrast dye, iodine, or shellfish.
- Arrive early to allow time for pre-procedure testing and preparation.
During the Procedure
- You’ll be awake but sedated (relaxed and comfortable but not unconscious).
- Local anesthetic will numb the catheter insertion area.
- Duration varies: angiogram alone typically takes 30–60 minutes; angioplasty may take 1–2 hours.
After the Procedure
- You’ll be monitored for a few hours for bleeding or complications.
- Most people can go home the same day, unless complications occur or the procedure is done as an emergency.
- Avoid strenuous activity or heavy lifting for a short period (usually 24–48 hours).
- Follow instructions on wound care and medications, especially blood thinners if you received a stent.
- Report chest pain, severe swelling, fever, or unusual symptoms to your care team immediately.
Frequently Asked Questions (FAQs)
Are angiogram and angioplasty painful?
Most patients experience little to no pain during the procedure. You may feel pressure when the catheter is inserted. With angioplasty, temporary discomfort or chest pressure can occur when the balloon is inflated, but this is brief and closely monitored.
How long is the recovery time?
Most people recover quickly, often returning to normal activities within a few days. If the procedure was emergent or complications developed, recovery may take longer.
Can a blockage come back after angioplasty?
Yes. While stents reduce the risk, the treated artery can narrow again (restenosis). Adhering to medications, managing your risk factors, and making lifestyle changes are crucial to preventing recurrence.
Are there alternatives to angioplasty?
Yes. Some blockages can be treated medically (medications, lifestyle changes), or with surgical options like coronary artery bypass grafting (CABG) for more extensive disease. Your doctor will recommend the best option based on your situation.
Do you always need a stent with angioplasty?
Not always, but it’s common. Stents help keep the artery open longer and reduce the chance of restenosis compared to balloon angioplasty alone.
Key Takeaways
- Angiograms are minimally invasive diagnostic tests that visualize the arteries.
- Angioplasty is a minimally invasive therapy that opens blocked arteries, often using stents.
- Both procedures are essential for diagnosing and treating coronary artery disease but serve unique purposes—one identifies, the other treats.
- Follow-up care, including medications and lifestyle improvements, is vital for sustaining heart health after these procedures.
If you’re faced with the possibility of either procedure, don’t hesitate to ask your cardiologist for information tailored to your personal situation. Informed patients are empowered patients.
References
- https://www.timelymedical.ca/angiogram-vs-angioplasty-key-differences/
- https://www.healthline.com/health/heart/angiogram-vs-angioplasty
- https://www.cardiaccarepc.com/content-hub/angiogram-vs-angioplasty-everything-you-need-to-know
- https://punecardiologist.com/blog/difference-between-angiogram-and-angioplasty.php
- https://www.medanta.org/patient-education-blog/what-is-the-difference-between-angioplasty-and-angiography
- https://sunnybrook.ca/content/?page=angiogram-angioplasty-heart-artery-video
- https://riversidebnj.com/angiogram-vs-angioplasty/
- https://www.dxnimble.com/angioplasty-vs-angiogram-what-is-the-difference/
Read full bio of Sneha Tete












