Angina vs. Coronary Artery Disease: Understanding the Key Differences
Explore how angina and coronary artery disease are connected, their distinctive symptoms, causes, and what sets them apart for better heart health.
Angina vs. Coronary Artery Disease: Key Differences Explained
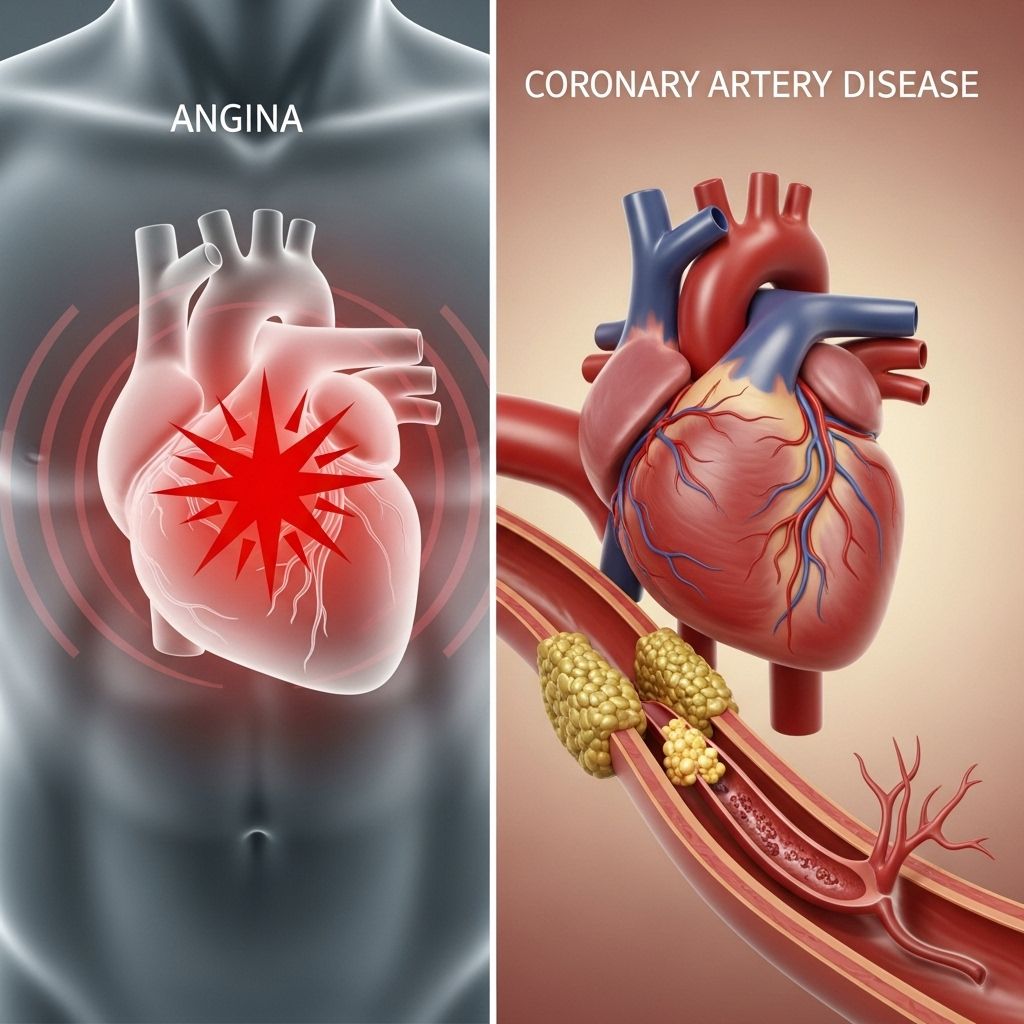
Understanding the connection and the differences between angina and coronary artery disease (CAD) is crucial for recognizing heart symptoms, assessing personal risk, and seeking timely medical care. While both relate to restricted blood flow to the heart muscle, they represent distinct heart conditions with unique symptoms, implications, and treatment approaches.
What Are Angina and Coronary Artery Disease?
Coronary artery disease is the most common type of heart disease. It occurs when plaque builds up inside the arteries that supply blood to the heart, narrowing or blocking the vessels and reducing blood flow. This buildup of plaque (made from cholesterol, fat, calcium, and other substances) over time is called atherosclerosis.
Angina, on the other hand, is not a disease but a symptom of coronary artery disease. It refers to the chest pain that happens when the heart muscle does not get enough blood and oxygen, typically due to these narrowed arteries.
- Angina: Chest pain or discomfort caused by reduced blood flow to the heart.
- Coronary Artery Disease: The underlying disease caused by plaque buildup in the heart’s arteries.
How Are Angina and CAD Connected?
Angina serves as a warning sign for CAD. Having angina means the heart is temporarily deprived of sufficient oxygen, alerting to underlying heart trouble. However, not everyone with CAD will experience angina; some may remain asymptomatic until the disease advances.
Types of Angina
Multiple forms of angina exist, each with varied triggers and clinical significance:
- Stable Angina: Most common type; typically occurs during physical exertion or emotional stress and responds to rest or medication. Pain is predictable in pattern and intensity.
- Unstable Angina: Emerges unpredictably and often at rest. Pain may be more intense, prolonged, and does not improve with rest or medication; signals a higher risk for heart attack and requires urgent medical intervention.
- Microvascular Angina: More common in women; results from poor function of small blood vessels in the heart and may not correlate with large artery blockages. Symptoms can be atypical such as fatigue or indigestion.
Symptoms: How to Tell Angina and CAD Apart
| Feature | Angina | Heart Attack (Result of Severe CAD) |
|---|---|---|
| Main Cause | Temporary decrease in blood flow to the heart | Permanent blockage (often due to plaque rupture or blood clot) |
| Chest Pain | Pressure, squeezing, burning, usually behind the breastbone | More intense, crushing pain; may radiate to arm, jaw, back |
| Duration | Few minutes; predictable, often with exertion | Longer duration; sudden onset, does not go away with rest |
| Relief | Improves with rest or nitroglycerin | No relief from rest or usual angina medication |
| Associated Symptoms | Shortness of breath, sweating, nausea (sometimes) | Nausea, vomiting, cold sweat, lightheadedness, extreme fatigue |
| Risk | Warning symptom of heart risk | Medical emergency; can lead to heart damage or death |
Typical Angina Symptoms
- Pressure, tightness, or pain in the chest—often central or left-sided
- Pain that may radiate to neck, jaw, shoulder, back, or arms
- Shortness of breath
- Burning or squeezing sensation behind the breastbone
- Indigestion-like feelings
- Symptoms triggered by physical activity, cold, or emotional stress
- Relieved by rest or nitroglycerin
Heart Attack Symptoms
- Severe chest pain or discomfort not relieved by rest
- Pain radiating more widely (e.g., left arm, back, jaw)
- Sweating, nausea, vomiting
- Sudden onset of weakness or extreme fatigue
- Shortness of breath at rest
- Cold sweat, dizziness, faintness
Note: Immediate emergency care is essential for heart attack symptoms, as delay increases risk of heart damage and death.
Who Is at Risk?
- People with risk factors for atherosclerosis (plaque buildup), including:
- High cholesterol and high blood pressure
- Smoking and excess alcohol consumption
- Diabetes
- Obesity, sedentary lifestyle
- Family history of heart disease
- Older age
- Stress and sleep disorders
- Women may experience atypical, flu-like symptoms of angina and heart attack (e.g., nausea, indigestion, fatigue)
Causes of Angina and CAD
CAD is driven by atherosclerosis, which develops from:
- High cholesterol and triglycerides
- High blood pressure
- Chronic inflammation
- Genetic factors
- Unhealthy diet high in saturated/trans fats
- Physical inactivity
- Smoking and excessive alcohol intake
Angina can be triggered by:
- Physical activity (walking, climbing stairs)
- Strong emotions or stress
- Cold weather
- Heavy meals
- Smoking
When to Seek Medical Care
Chest pain—especially if new, worsening, or occurring at rest—should always be evaluated by a healthcare professional. Call emergency services if you experience:
- Chest pain lasting more than a few minutes
- Pain radiating to the arm, neck, jaw, or back
- Shortness of breath, sweating, nausea, or fainting
- Sudden, intense fatigue or weakness
Angina often requires medical management, but unstable angina or suspected heart attack requires immediate attention.
Diagnosing Angina and Coronary Artery Disease
Doctors diagnose angina and CAD using:
- Medical history and physical examination
- Electrocardiogram (ECG): Looks for heart rhythm and damage
- Stress testing: Assesses heart’s response to exercise
- Coronary angiography: Imaging test to view artery blockages
- Blood tests: Detect markers of heart damage
- Cardiac CT or MRI: Advanced imaging for structure and function
Diagnosis guides treatment and risk assessment for heart attacks and other complications.
Treatment Options
Options depend on the severity and type of heart issue.
| Treatment | Angina | Coronary Artery Disease |
|---|---|---|
| Medications | Nitroglycerin, beta blockers, calcium channel blockers, statins | Statins, anti-hypertensives, antiplatelets, diabetes management |
| Lifestyle Changes | Smoking cessation, weight loss, stress reduction, exercise, heart-healthy diet | Same as above; critical for long-term management |
| Procedures | If medication fails, angioplasty or stent placement may be needed | Angioplasty, stents, or coronary artery bypass grafting (CABG) |
- Stable angina often managed with medications and lifestyle changes.
- Unstable angina and heart attacks may require emergency stenting or surgery to restore blood flow.
- Advanced CAD may need surgical intervention like bypass surgery.
Preventing Angina and CAD
Many risk factors are modifiable. Steps to reduce risk include:
- Quit smoking
- Eat a diet low in saturated fat, high in vegetables and whole grains
- Exercise regularly
- Maintain healthy blood pressure, cholesterol, and weight
- Manage stress and sleep disorders
- Monitor blood sugar in diabetes
- Attend regular checkups if you are at risk or have heart symptoms
Frequently Asked Questions (FAQ)
Q: Is angina the same as a heart attack?
A: No. Angina is chest pain from reduced blood flow to the heart, serving as a warning symptom. A heart attack is permanent damage to heart muscle due to a complete and sustained blockage.
Q: How do I know if my chest pain is angina or a heart attack?
A: Angina often occurs with exertion and improves with rest or medication. Heart attack pain is more severe, lasts longer, and does not improve with rest. If you are unsure, seek medical attention immediately.
Q: Can angina lead to a heart attack?
A: Yes. Angina may indicate underlying coronary artery disease and a higher risk for heart attack. Unstable angina especially can signal imminent risk.
Q: Are symptoms different in men and women?
A: Women may have more subtle symptoms such as fatigue, nausea, indigestion, or muscle aches rather than classic chest pain. These can be mistakenly attributed to less serious health issues.
Q: What should I do if I have angina symptoms?
A: Rest and take prescribed medication. If symptoms worsen, last longer, or occur at rest, seek emergency care as this could signal a heart attack or unstable angina.
Q: Can lifestyle changes reverse coronary artery disease?
A: While lifestyle changes can slow progression, improve symptoms, and sometimes help partially reverse plaque buildup, advanced disease often requires medical or surgical intervention.
Summary
Angina is a symptom of coronary artery disease, caused by restricted blood supply to the heart. CAD is the underlying disease process resulting from plaque buildup. Angina episodes signal potential risk and should always be discussed with a healthcare provider. Understanding the differences, recognizing warning signs, and adopting preventive measures are essential for optimal heart health.
References
- https://www.goodrx.com/conditions/coronary-artery-disease/heart-attack-vs-angina
- https://www.heartscope.com.au/what-is-the-difference-between-angina-and-a-heart-attack/
- https://www.midgaheart.com/blog/whats-the-difference-between-a-heart-attack-and-angina/
- https://www.thecardiologyadvisor.com/features/angina-vs-heart-attack/
- https://www.mayoclinic.org/diseases-conditions/angina/symptoms-causes/syc-20369373
- https://www.nhlbi.nih.gov/resources/know-differences-cardiovascular-disease-heart-disease-coronary-heart-disease
- https://www.heartfoundation.org.nz/your-heart/heart-conditions/angina
- https://pubmed.ncbi.nlm.nih.gov/34555447/
Read full bio of medha deb












