Angina Pectoris: Causes, Symptoms, Diagnosis, and Treatment
Understand angina pectoris—its symptoms, risk factors, how it’s diagnosed, management options, and life with this heart condition.
Angina Pectoris
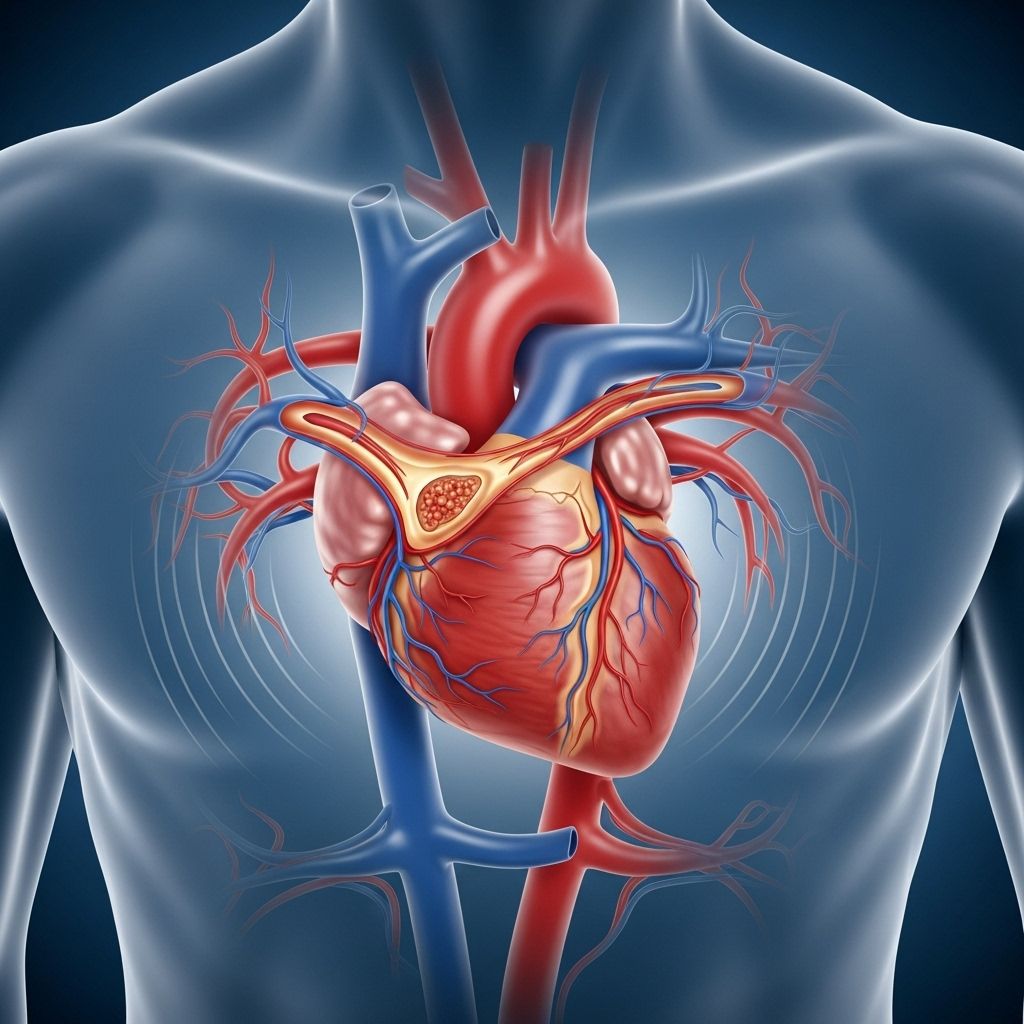
Angina pectoris, commonly referred to as angina, describes chest pain or discomfort occurring when an area of the heart muscle does not receive enough oxygen-rich blood. It is often a warning sign of underlying heart problems, most frequently coronary artery disease (CAD).
What Is Angina Pectoris?
Angina pectoris is the result of a temporary shortage in oxygen supply to the heart muscle. While it does not usually cause permanent heart damage, it almost always signals a higher risk for more serious heart issues, including heart attacks. Recognizing and treating angina is important for maintaining long-term cardiac health.
Types of Angina
Several distinct forms of angina exist, distinguished by their causes and symptoms:
- Stable Angina: The most common type, triggered by physical activity or emotional stress and usually relieved by rest or medication.
- Unstable Angina: More unpredictable, can occur at rest, does not follow a regular pattern, and signals a higher risk of heart attack. Medical attention is needed immediately.
- Microvascular Angina (formerly Syndrome X): Chest pain occurs even without coronary artery blockage, caused by poor function of tiny blood vessels. Seen more often in women.
- Variant (Prinzmetal’s) Angina: Rare type caused by temporary spasm in a coronary artery, typically occurs at rest and may be very severe. Not associated with plaque build-up.
Causes of Angina Pectoris
Most often, angina results from coronary artery disease, where the blood supply to heart muscle is restricted by narrowing or blockage in the coronary arteries, usually due to:
- Atherosclerosis: Hardening and narrowing of arteries from plaque buildup.
- Blood Clot: Can suddenly block a narrowed artery, leading to symptoms.
- Poor blood flow through a narrowed heart valve (e.g., aortic stenosis).
- Reduced pumping strength of the heart muscle.
- Coronary artery spasm: Temporary narrowing due to muscular spasms.
In some circumstances, angina is caused by “unstable plaque”—plaques that rupture and trigger clotting, reducing or blocking blood supply. Other triggers can include anemia, rapid heartbeat, or high blood pressure, all of which can increase the heart’s oxygen demand.
Who Is at Risk?
Anyone can be affected by angina, but certain risk factors make it more likely, such as:
- Age (risk increases after age 45 for men, 55 for women)
- Family history of heart disease
- High blood pressure (hypertension)
- High cholesterol levels
- Diabetes
- Obesity or overweight
- Smoking
- Physical inactivity
- Unhealthy diet high in saturated fats and sugars
- Chronic stress
Symptoms of Angina
The hallmark symptom of angina is chest pain or discomfort, though the experience can vary between individuals. Key observations include:
- Sensation: May feel like pressure, squeezing, fullness, burning, tightness, or pain in the chest.
- Location: Usually behind the breastbone but can radiate to shoulders, arms, neck, jaw, or back.
- Other symptoms: Shortness of breath, sweating, nausea, fatigue, dizziness, or lightheadedness.
- Duration: Typically lasts a few minutes, subsides with rest or medication (especially nitroglycerin).
- Triggers: Physical exertion, emotional stress, heavy meals, cold weather, or smoking.
Women, older adults, and people with diabetes may have less typical symptoms, such as shortness of breath, nausea, abdominal pain, or fatigue, rather than classic chest pain.
Diagnosing Angina
Early, accurate diagnosis is critical. Healthcare providers use a combination of medical history, physical examination, and diagnostic tests to confirm angina:
- Medical history and symptom review: Identifying triggers, pattern, and associated symptoms.
- Physical exam: May reveal clues to heart function or other health problems.
- Electrocardiogram (ECG or EKG): Records electrical activity of the heart to detect areas with reduced blood supply or past heart attack.
- Stress testing: The heart is monitored during exercise or medication-induced stress to uncover symptoms or ECG changes.
- Echocardiogram: Ultrasound imaging evaluates heart structure and pumping ability.
- Blood tests: Assess cholesterol levels, markers of heart damage, and diabetes.
- Cardiac catheterization and angiography: Invasive test using X-ray and contrast dye to visualize blockages in coronary arteries.
- CT and MRI scans: Advanced imaging for structural and blood flow assessment.
Complications of Angina
Angina suggests a higher risk for life-threatening heart conditions, including:
- Heart attack (myocardial infarction): Prolonged or severe reduction in blood supply can permanently damage heart muscle.
- Arrhythmias: Abnormal heart rhythms may arise, particularly in individuals with significant coronary artery disease.
- Heart failure: Repeated or severe angina can weaken the heart over time.
When to Seek Emergency Help
If you have chest pain you have not experienced before, or if usual angina symptoms suddenly become worse, more frequent, or occur at rest, seek immediate medical attention. Quick action is crucial, as these symptoms may indicate a heart attack or unstable angina.
Treatment Options for Angina
Treatment aims to relieve symptoms, prevent angina attacks, improve quality of life, and decrease the risk of heart attack and cardiac death. A multi-faceted approach is often necessary:
Lifestyle Changes
- Adopt a heart-healthy diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats.
- Engage in regular physical activity as recommended by your healthcare provider.
- Quit smoking and avoid exposure to secondhand smoke.
- Achieve and maintain a healthy weight.
- Manage stress through relaxation techniques, therapy, or mindfulness.
- Control medical conditions such as high blood pressure, diabetes, and high cholesterol.
Medications
| Medication | Role/Mechanism |
|---|---|
| Nitrates (e.g., Nitroglycerin) | Dilates blood vessels, improves heart’s oxygen supply, used for quick relief and prevention of symptoms. |
| Beta Blockers | Slows heart rate, lowers blood pressure, reduces heart’s oxygen demand. |
| Calcium Channel Blockers | Relaxes blood vessels and heart muscle, lowers blood pressure, alternative or addition to beta blockers. |
| Aspirin | Prevents blood clots, reduces risk of heart attack and stroke; do not take daily aspirin without supervision. |
| Statins | Lowers cholesterol, may reduce inflammation and stabilize arterial plaques. |
| ACE Inhibitors | Relaxes blood vessels, reduces blood pressure and work required from your heart. |
| Ranolazine | Decreases heart’s oxygen demand, used when other medicines are insufficient. |
Never take erectile dysfunction medications (such as sildenafil, vardenafil, or tadalafil) with nitroglycerin, as this combination can cause dangerous drops in blood pressure.
Procedures and Surgery
- Angioplasty and Stenting: A catheter with a small balloon is threaded to blocked coronary arteries, inflated to open them, then a stent is placed to keep the artery open.
- Coronary Artery Bypass Graft (CABG) Surgery: Surgeons use blood vessels from other parts of the body to create a new path for blood to bypass severely narrowed or blocked arteries, restoring proper flow to the heart muscle.
Living with Angina
With proper management, most people with angina can engage in normal activities and have a good quality of life. Effective strategies to manage angina include:
- Understanding your triggers and learning to avoid or manage them.
- Carrying prescribed nitroglycerin at all times if indicated.
- Adhering to medications as directed by your healthcare team.
- Maintaining healthy lifestyle habits for the long term.
- Scheduling regular check-ups and keeping your healthcare team informed of any changes in symptoms or new health issues.
Prevention
- Eat a nutritious, low-sodium diet with minimal saturated and trans fats.
- Exercise regularly according to ability and guidance.
- Avoid tobacco and limit alcohol use.
- Keep stress under control and rest adequately.
- Monitor and manage blood pressure, cholesterol, and blood sugar.
Frequently Asked Questions (FAQs)
Q: What does angina typically feel like?
A: Most people describe angina as chest pain, tightness, squeezing, or pressure. It may radiate to the arms, neck, jaw, or back, and be associated with shortness of breath or fatigue.
Q: Can you have angina without chest pain?
A: Yes. Some people, especially women, older adults, and those with diabetes, may experience angina as breathlessness, nausea, discomfort in the back or jaw, or unusual fatigue rather than typical chest pain.
Q: How is angina diagnosed?
A: Angina is diagnosed using a combination of history, physical exam, ECG, stress testing, blood tests, and heart imaging studies to determine if the heart muscle is short of blood or has underlying disease.
Q: Is all chest pain caused by angina?
A: No. Chest pain can be due to digestive issues, lung disease, muscle strain, or anxiety, among others. Angina is just one cause and should be evaluated especially if you have risk factors for heart disease.
Q: What should I do if I suspect I have angina?
A: Any new, unexpected, or worsening chest pain should be assessed by a healthcare professional immediately, as it may signal a heart attack or other urgent condition.
Summary Table: Types of Angina
| Type | Triggers/Features | Management |
|---|---|---|
| Stable Angina | Exertion or stress; predictable; relieves with rest/medication | Lifestyle changes, medications |
| Unstable Angina | At rest or minimal exertion; unpredictable; does not improve with rest | Emergency care, possible procedures |
| Variant (Prinzmetal’s) Angina | Coronary artery spasm; often at rest, early morning/night | Medications (e.g., calcium channel blockers, nitrates) |
| Microvascular Angina | No major artery blockage; involves small vessels | Medications, lifestyle changes |
Key Takeaways
- Angina is a symptom—not a disease itself—signaling reduced blood flow to the heart muscle.
- Effective diagnosis and treatment can reduce symptoms, prevent complications, and improve quality of life.
- Recognizing risk factors and early warning signs is crucial for prompt care.
- Adopting healthy habits is paramount for prevention and management of angina.
References
- https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=85&ContentID=P00194
- https://www.health.harvard.edu/heart-health/angina-symptoms-diagnosis-and-treatments
- https://www.mayoclinic.org/diseases-conditions/angina/diagnosis-treatment/drc-20369378
- https://my.clevelandclinic.org/health/diseases/21489-angina
- https://www.mayoclinic.org/diseases-conditions/angina/symptoms-causes/syc-20369373
- https://www.nhs.uk/conditions/angina/
- https://www.massgeneralbrigham.org/en/patient-care/services-and-specialties/heart/conditions/angina
- https://www.nhlbi.nih.gov/health/angina/treatment
- https://www.bhf.org.uk/informationsupport/conditions/angina
Read full bio of Sneha Tete












