Understanding the Link Between Anemia and Heart Failure
Explore how anemia and heart failure intersect, impact health, and what can be done to manage both conditions effectively.
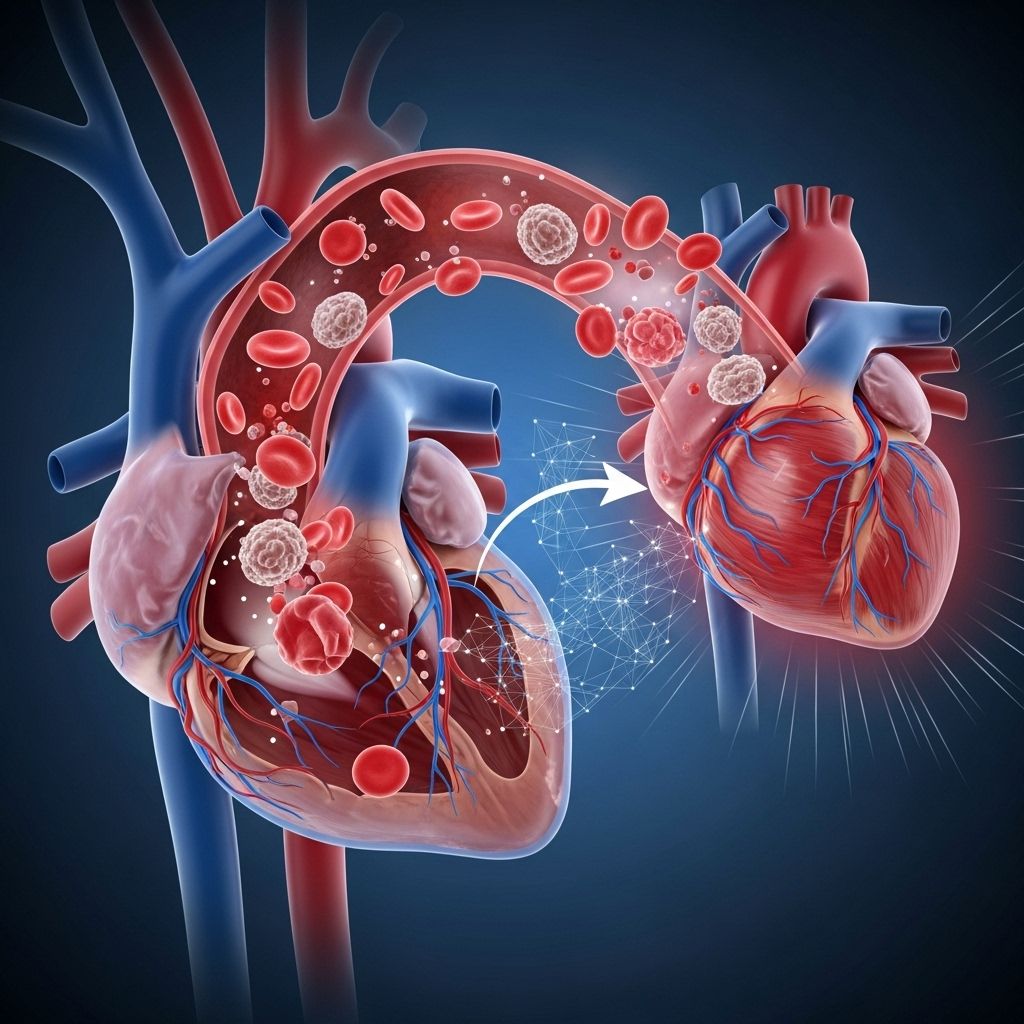
Anemia and Heart Failure: Understanding the Connection
Anemia and heart failure are two distinct yet frequently intertwined medical conditions. Their coexistence creates a complex clinical challenge, often resulting in worse outcomes for affected individuals. This article explores the interplay between anemia and heart failure, including causes, risk factors, clinical significance, diagnosis, management, and tips for living with these chronic health issues.
What Is Anemia?
Anemia is a condition characterized by a deficiency of healthy red blood cells or hemoglobin in the blood. This deficiency results in reduced oxygen delivery to the body’s organs and tissues, leading to fatigue and other health problems. Anemia is commonly recognized by a hemoglobin concentration of less than 13 g/dL in men and less than 12 g/dL in women.
- Hemoglobin: The oxygen-carrying protein in red blood cells.
- Red Blood Cells: Cells responsible for transporting oxygen from the lungs to tissues throughout the body.
- Iron Deficiency: The most common cause of anemia, especially in chronic disease states.
What Is Heart Failure?
Heart failure is a chronic condition in which the heart’s ability to pump blood effectively is impaired. This can cause fluid buildup in the lungs, legs, and other tissues, resulting in symptoms such as shortness of breath, fatigue, and swelling. Heart failure may be classified based on the heart’s ejection fraction, the amount of blood the heart pumps with each beat:
- Heart failure with reduced ejection fraction (HFrEF)
- Heart failure with preserved ejection fraction (HFpEF)
How Are Anemia and Heart Failure Linked?
Anemia and heart failure have a bidirectional relationship, each potentially worsening the other. Anemia is common in individuals with heart failure, particularly in those with advanced disease, and its presence correlates with increased morbidity and mortality.
- Prevalence:
- Occurs in roughly 30% of patients with stable heart failure
- Seen in up to 50% of hospitalized heart failure patients
- Much higher than in the general population (less than 10%)
To effectively tackle the challenges of both conditions, it's crucial to manage anemia and diabetes together. This integrated approach not only addresses the symptoms but also aligns lifestyle changes that can enhance your quality of life. Learn more about strategies that can significantly impact your health journey. - Impact: Associated with older age, female gender, diabetes, chronic kidney disease (CKD), more severe heart failure, and poorer quality of life.
| Population | Prevalence of Anemia |
|---|---|
| General population | <10% |
| Stable heart failure | ~30% |
| Hospitalized heart failure | 40-50% |
Why Does Anemia Occur in Heart Failure?
Several mechanisms underlie the development of anemia in people with heart failure:
- Iron deficiency: Due to chronic blood loss, insufficient dietary intake, or poor intestinal absorption from gut edema.
- Chronic inflammation: Heart failure triggers chronic systemic inflammation, increasing levels of cytokines like TNF-alpha and IL-6, which suppress red blood cell production and alter iron metabolism.
- Chronic kidney disease (CKD): Reduced erythropoietin (EPO) production impairs the body’s ability to make red blood cells.
- Medication effects: Drugs such as ACE inhibitors and angiotensin receptor blockers (ARBs), as well as certain diuretics, can contribute to anemia by reducing EPO production or causing nutrient loss.
- Malnutrition and blood loss: Poor nutritional status and gastrointestinal bleeding, common in advanced heart failure, further increase anemia risk.
Symptoms: How Anemia and Heart Failure Can Overlap
Many symptoms of anemia and heart failure are similar, making diagnosis challenging without laboratory confirmation.
- Fatigue and weakness
- Shortness of breath, especially on exertion
- Reduced exercise tolerance
- Rapid or irregular heartbeat
- Swelling in the legs or abdomen
- Pale or yellowish skin
Risks of Having Both Anemia and Heart Failure
The coexistence of these conditions intensifies health risks:
- Increased hospitalizations
- Higher mortality rates (anemia doubles risk of death in heart failure patients)
- Poorer functional status and reduced quality of life
- Episodic worsening of both conditions during acute illness
Causes: Why Do Anemia and Heart Failure Occur Together?
There are interconnected causes behind this association:
- Cardiorenal syndrome: The heart and kidneys closely interact; heart failure often leads to kidney dysfunction, decreasing EPO production and exacerbating anemia.
- Chronic inflammation: Heart failure promotes inflammation, altering the environment of bone marrow and impairing the body’s use of iron for red blood cell production.
- Hormonal changes: Overactivation of the renin-angiotensin-aldosterone system results in sodium and water retention, further stressing heart and kidneys.
Iron Deficiency: The Most Common Cause
Among heart failure patients, iron deficiency is the most frequent cause of anemia. Chronic heart failure affects iron distribution and absorption:
- Chronic inflammatory state increases hepcidin, a hormone that reduces intestinal iron absorption and keeps iron locked in storage sites.
- Edema (swelling) of the gut wall impairs absorption of nutrients, including iron.
Diagnosis: How Are Anemia and Heart Failure Detected?
Diagnosing anemia in patients with heart failure involves a multi-step process:
- Blood Tests: Evaluation of hemoglobin and hematocrit levels reveals anemia. Additional markers like mean corpuscular volume (MCV), iron levels, ferritin, and transferrin saturation help determine the type.
- Assessing Iron Status: Low iron and ferritin levels indicate iron deficiency; a high ferritin with low transferrin saturation suggests functional iron deficiency and inflammation as the cause.
- Assessing Kidney Function: Measuring BUN, creatinine, and estimated glomerular filtration rate (eGFR) establishes CKD involvement.
- Underlying Causes: Screening for gastrointestinal bleeding, dietary deficiencies, or medication effects may be necessary.
| Test | Role |
|---|---|
| Hemoglobin | Confirms anemia |
| Hematocrit | Assesses severity |
| Ferritin | Reflects iron stores (interpret with caution in inflammation) |
| Transferrin saturation | Indicates available iron for use |
| Serum iron | Low in deficiency or chronic disease |
| Creatinine/eGFR | Assesses kidney involvement |
Management: Treatment of Anemia in Heart Failure
The management of anemia in heart failure focuses on correcting reversible factors, improving quality of life, and reducing hospitalizations. Treatment is tailored to the underlying cause:
- Iron Supplementation
- Intravenous (IV) iron is preferred for heart failure patients, especially when oral absorption is impaired or ineffective.
- Studies show improvement in symptoms, exercise tolerance, and hospitalizations with IV iron in those with true iron deficiency.
- Erythropoiesis-Stimulating Agents (ESAs)
- Initially considered for those with heart failure and CKD, but clinical trials found little to no benefit in reducing morbidity or mortality.
- Latest guidelines recommend against routine ESA use in heart failure.
- Treating Underlying Causes
- Addressing gastrointestinal bleeding, dietary deficiencies, and medication side effects is essential.
- Managing comorbidities like diabetes and CKD improves overall outcomes.
- Red Blood Cell Transfusions
- Reserved for severe, symptomatic anemia or acute bleeding.
- Not recommended for stable chronic anemia due to potential complications.
Monitoring and Follow-Up
Ongoing monitoring of blood counts, iron status, and kidney function helps guide therapy and prevent recurrence. Regular assessments ensure timely modification of treatment plans based on individual response and disease progression.
Potential Complications and Prognosis
- Poor exercise tolerance and reduced quality of life.
- Higher risk of adverse cardiac events, hospitalization, and death.
- Persistent or worsening anemia can indicate disease progression or inadequate management.
Living With Anemia and Heart Failure
Managing both anemia and heart failure requires a comprehensive, proactive approach. Here are some important considerations:
- Follow medication regimens and attend all scheduled appointments.
- Monitor symptoms: Changes in energy, breathing, or swelling should be reported promptly.
- Maintain a balanced diet with adequate iron, vitamin B12, and folate (as recommended by your healthcare provider).
- Manage other chronic conditions such as CKD or diabetes aggressively.
- Stay physically active as tolerated and approved by your healthcare provider.
Summary Table: Key Facts About Anemia and Heart Failure
| Aspect | Details |
|---|---|
| Prevalence in HF | 30–50% depending on setting |
| Main Causes | Iron deficiency, CKD, chronic inflammation, poor nutrition |
| Main Risks | Higher mortality, more hospitalizations, worse symptoms |
| Best Diagnostic Tools | Hemoglobin, iron studies, kidney function tests |
| Preferred Treatment | IV iron for iron deficiency; avoid routine ESAs and transfusions |
| Patient Self-Care | Symptom monitoring, adequate nutrition, adherence to treatment |
Frequently Asked Questions (FAQs)
Q: Can treating anemia improve my heart failure symptoms?
A: Treating iron deficiency—especially with intravenous iron—has been shown to improve exercise tolerance and relieve some symptoms in people with both heart failure and anemia. However, it does not reduce overall mortality.
Q: Why shouldn’t I just take over-the-counter iron supplements?
A: In heart failure, especially with gut swelling or chronic inflammation, oral iron may not be well-absorbed or effective, and unsupervised supplementation can cause side effects. Always consult your doctor before starting any supplement.
Q: Is anemia always caused by iron deficiency in heart failure?
A: Iron deficiency is the most common cause, but anemia in heart failure can also arise from chronic kidney disease, inflammation, certain medications, and nutritional deficiencies. Proper diagnosis is vital.
Q: Are blood transfusions safe for heart failure patients?
A: Blood transfusions are usually reserved for severe or rapidly worsening anemia. In chronic, stable cases, transfusions carry risks and are not routinely recommended.
Q: What should I ask my doctor if I have both conditions?
A: Ask about your hemoglobin and iron levels, possible causes of your anemia, the best treatment options in your case, and how to monitor your symptoms during therapy.
Takeaway
Anemia and heart failure often coexist, significantly impacting quality of life and health outcomes. Recognizing their interplay is essential for optimal management. Timely diagnosis, appropriate treatment, and proactive self-care can help reduce symptom burden and improve daily functioning for those managing both conditions.
References
- https://www.ahajournals.org/doi/10.1161/circulationaha.118.030099
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9393312/
- https://pubmed.ncbi.nlm.nih.gov/15593047/
- https://www.acc.org/Latest-in-Cardiology/Articles/2021/07/06/12/18/Anemia-and-Heart-Failure
- https://www.ahajournals.org/doi/10.1161/circ.150.suppl_1.4141968
Read full bio of medha deb












