Anatomy of the Female Pelvic Area: Structures, Functions, and Common Disorders
A comprehensive guide to the female pelvic anatomy, its functions, and common conditions affecting women across the lifespan.
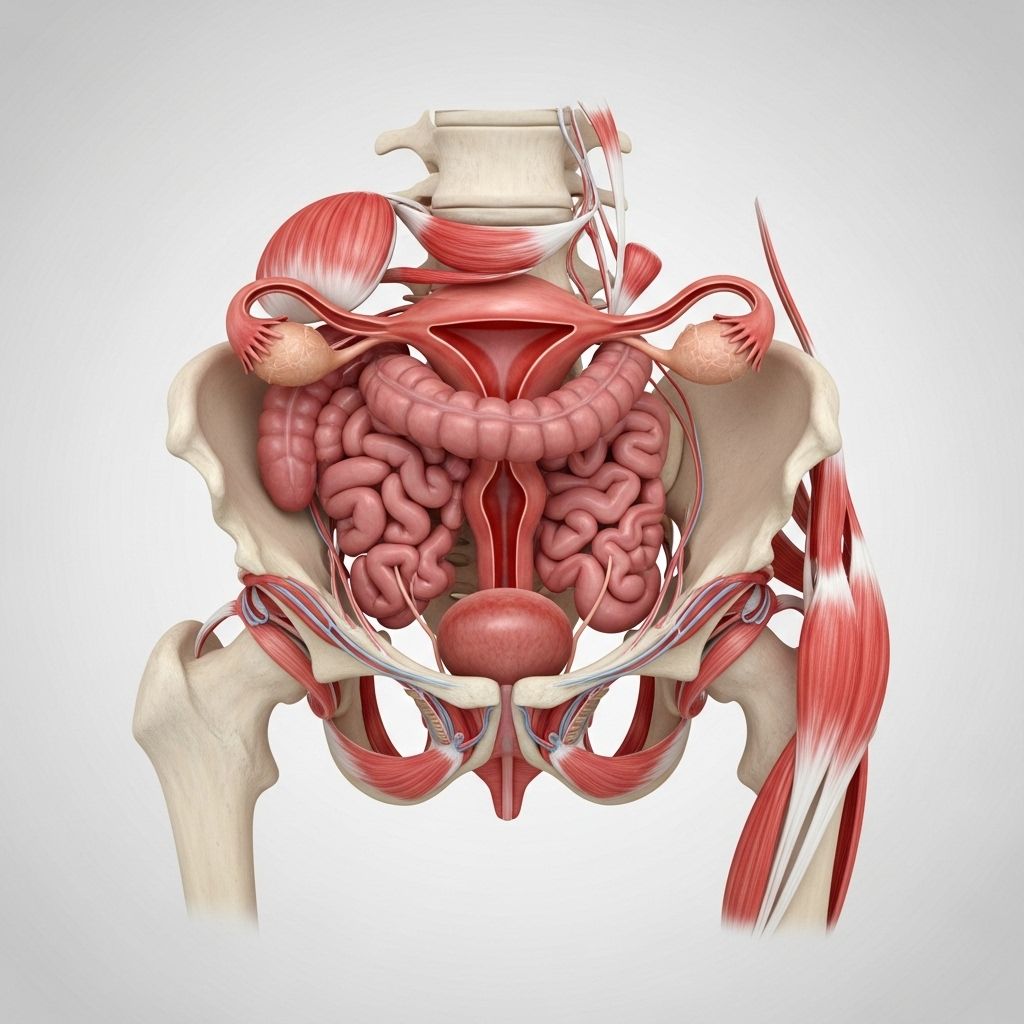
Anatomy of the Female Pelvic Area
The female pelvic area is a complex region containing vital organs, muscles, ligaments, and blood vessels. Its unique structure supports reproductive, urinary, bowel, and muscular functions critical to a woman’s health throughout life. Understanding this anatomy improves prevention and management of common pelvic conditions.
What Is the Female Pelvis?
The pelvis is a basin-shaped structure formed by bones, muscles, and ligaments. It houses and protects reproductive, urinary, and bowel organs, provides attachment sites for muscles, and supports the body’s weight during sitting, standing, and walking.
- Bony boundaries: Composed of the hip bones (ilium, ischium, pubis), sacrum, and coccyx.
- Pelvic cavity: Divided into a false (greater) pelvis above, and a true (lesser) pelvis below, which contains most pelvic organs.
Main Organs and Structures
The female pelvic area contains several core organs and structures, each with a distinct function:
- Reproductive organs: Uterus, ovaries, fallopian tubes, and vagina.
- Urinary system: Bladder and urethra.
- Bowel structures: Rectum and part of the large intestine.
- Muscles and ligaments: Pelvic floor muscles, ligaments that stabilize organs.
Major Organs of the Female Pelvic Area
Uterus
The uterus is a hollow, muscular organ located centrally in the pelvis. It is pear-shaped and serves as the site for fetal development during pregnancy.
- Parts:
- Fundus: Top, dome-shaped portion above the fallopian tubes.
- Corpus (body): Central, largest part.
- Cervix: Lower narrow portion opening into the vagina.
- Functions: Monthly menstruation, implantation site for embryo, contracts during childbirth.
Ovaries
The ovaries are two almond-shaped glands on either side of the uterus. They produce eggs (ova) and hormones (estrogen and progesterone).
- Size: About 3–5 cm in length.
- Functions: Release eggs for fertilization, regulate menstrual cycle, maintain hormone balance.
Fallopian Tubes
The fallopian tubes connect the ovaries to the uterus and are critical for transporting eggs and fertilization.
- Length: Approximately 7–12 cm each.
- Parts:
- Interstitial: Passes through uterine wall.
- Isthmus: Narrow segment near uterus.
- Ampulla: Wide, convoluted mid-section, typical site of fertilization and ectopic pregnancies.
- Infundibulum: Funnel-shaped, opens near ovary.
Vagina
The vagina is a muscular canal extending from the cervix to the vulva, serving as the passage for menstrual flow, intercourse, and childbirth.
- Length: About 8–10 cm.
- Functions: Birth canal, outlet for menstruation, receptacle during sexual activity.
Bladder and Urethra
The bladder is a hollow organ for urine storage, positioned just behind the pubic bone. The urethra runs a short course from the bladder to the vulva, enabling urination.
- Bladder location: Anterior aspect of the pelvis, anterior to the vagina.
- Support structures: Urogenital diaphragm, pubourethral ligaments.
- Urethral function: Conducts urine outside the body; pelvic floor muscles assist continence.
Rectum
The rectum is the terminal segment of the large intestine, located just behind the vagina and uterus. It stores and evacuates stool during defecation.
Muscles and Support Structures
The Pelvic Floor
The pelvic floor is a group of muscles and connective tissue spanning the bottom of the pelvis. These muscles provide critical support for pelvic organs, maintain continence, and contribute to sexual function.
- Main muscles:
- Levator ani (including pubococcygeus, puborectalis, iliococcygeus)
- Coccygeus muscle
- Additional structures: Perineal membrane, perineal body
- Innervation: Pudendal nerve (main), ilioinguinal and genitofemoral nerves (anterior)
- Functions:
- Support pelvic organs
- Regulate bladder and bowel function
- Assist in childbirth and sexual function
Ligaments and Connective Tissue
Several key ligaments help anchor and stabilize organs in the pelvic area:
- Cardinal ligaments: Stabilize pelvic organs horizontally.
- Uterosacral ligaments: Attach the cervix and uterus to the sacrum, providing deep pelvic support.
- Round ligament: Helps maintain uterine position.
- Pubourethral ligaments: Anchor proximal urethra to pubic bone, supporting the bladder and continence.
Blood Supply and Nerves
Pelvic organs receive blood from branches of the internal iliac artery and abdominal aorta. Nerves from the sacral plexus provide motor and sensory input for vulvar and pelvic functions.
- Main arteries: Internal iliac artery branches (uterine, vaginal, rectal arteries), external iliac becoming femoral artery.
- Nerve supply: Pudendal nerve (primary), ilioinguinal, genitofemoral, and pelvic splanchnic nerves.
External Genitalia of the Female Pelvis
Vulva
The vulva refers to the external genital structures including:
- Labia majora: Outer folds, protect inner structures.
- Labia minora: Inner folds, surround the urethra and vaginal openings.
- Clitoris: Erectile tissue structure, sensitive to stimulation.
- Vestibule: Area containing the openings of the urethra and vagina.
- Glands: Skene’s glands (near urethra), Bartholin’s glands (near vaginal opening).
Common Disorders Affecting the Female Pelvic Area
Pelvic Floor Dysfunction
Disorders of the pelvic floor muscles and connective tissue may lead to a variety of symptoms affecting urinary, bowel, and sexual function.
- Urinary incontinence: Leakage due to weakened support (e.g., stress incontinence).
- Fecal incontinence: Difficulty controlling bowel movements.
- Pelvic organ prolapse: Descent of the bladder, uterus, or bowel into or through the vaginal canal.
- Pelvic pain: Pain during intercourse or chronic pelvic discomfort.
Prolapse Conditions
Pelvic organ prolapse occurs when the support structures (muscles, ligaments) fail, allowing organs to drop:
- Cystocele: Bladder prolapses into the vagina.
- Rectocele: Rectum bulges into the vagina.
- Uterine prolapse: Uterus descends downward.
Why Does Pelvic Floor Dysfunction Occur?
- Pregnancy and childbirth (especially multiple deliveries or large babies)
- Heavy lifting or sustained high intra-abdominal pressure
- Aging and loss of estrogen
- Chronic respiratory illness requiring frequent coughing
- Obesity
- Pelvic injury or surgery
Other Common Issues
- Endometriosis: Uterine tissue grows outside the uterus causing pain and infertility.
- Ectopic pregnancy: Pregnancy occurs in the fallopian tube (most common in the ampulla), which can cause pain and internal bleeding.
- Ovarian torsion: Twisting of the ovary that may compromise blood supply; usually requires emergency treatment.
Diagnosing and Treating Pelvic Disorders
Pelvic floor disorders are often diagnosed through clinical examination and may involve imaging (ultrasound, CT, MRI), urodynamic testing, or surgical exploration. Treatment options depend on symptoms and severity.
- Physical therapy targeting pelvic floor muscles
- Medication for pain, inflammation, or infection
- Surgical repair for prolapse or severe incontinence
- Lifestyle modifications: Weight management, avoiding heavy lifting, smoking cessation
Table: Overview of Female Pelvic Organs and Their Functions
| Organ | Location | Main Function |
|---|---|---|
| Uterus | Central pelvis, above vagina | Fetal growth, menstruation |
| Ovaries | Side of uterus | Egg, hormone production |
| Fallopian tubes | Between ovaries and uterus | Transport eggs, fertilization site |
| Vagina | From cervix to vulva | Birth canal, menstruation, intercourse |
| Bladder | Anterior pelvis | Store urine |
| Rectum | Posterior pelvis | Store and evacuate stool |
Preserving Pelvic Health
- Kegel exercises: Strengthen pelvic floor muscles, helping support organs and improve continence.
- Good posture and exercise: Support strong muscles and ligaments.
- Timely treatment for infections: Prevents complications.
- Regular checkups: Enables early diagnosis of common disorders.
Frequently Asked Questions (FAQs)
Q: What are the most important pelvic floor muscles in women?
A: The levator ani group—pubococcygeus, puborectalis, and iliococcygeus—plus the coccygeus are crucial for pelvic support, continence, and reproductive functions.
Q: What symptoms indicate pelvic floor dysfunction?
A: Symptoms include urine or stool leakage, a feeling of vaginal bulging, pelvic pain, inability to empty bladder, pain with intercourse, and lower back discomfort.
Q: How is pelvic organ prolapse treated?
A: Mild prolapse may be managed with pelvic floor exercises, physical therapy, or pessaries. Severe cases might need surgical repair to restore support.
Q: How does pregnancy affect the pelvic area?
A: Pregnancy stretches pelvic muscles and ligaments and increases pressure, sometimes leading to weakness or prolapse, especially after multiples or large babies.
Q: Why is the ampulla of the fallopian tube important?
A: The ampulla is the most common site for ectopic pregnancies because it can expand more than other segments and is the typical site for egg fertilization.
Q: Does pelvic anatomy change as women age?
A: Yes, loss of estrogen, weakening of support structures, and thinning of soft tissues can increase risk for incontinence and prolapse over time.
Quick Facts: Anatomy of Female Pelvic Area
- The female pelvis holds reproductive, urinary, and bowel organs critical to overall health.
- Muscles, ligaments, and nerves provide support and functional control.
- Common problems include prolapse, incontinence, chronic pain, and gynecologic disease.
- Early intervention, targeted exercises, and surgical options improve outcomes.
References
- https://www.youtube.com/watch?v=z71sBzXZBpI
- https://pubmed.ncbi.nlm.nih.gov/2017803/
- https://www.youtube.com/watch?v=W_IowldPRSQ
- https://pure.johnshopkins.edu/en/publications/current-concepts-of-female-pelvic-anatomy-and-physiology-4
- https://pure.johnshopkins.edu/en/publications/current-concepts-of-female-pelvic-anatomy-and-physiology-4/fingerprints/
Read full bio of Sneha Tete












