Anatomy and Function of the Coronary Arteries
A comprehensive exploration of the coronary arteries, their critical function, anatomy, and their crucial role in cardiovascular health.
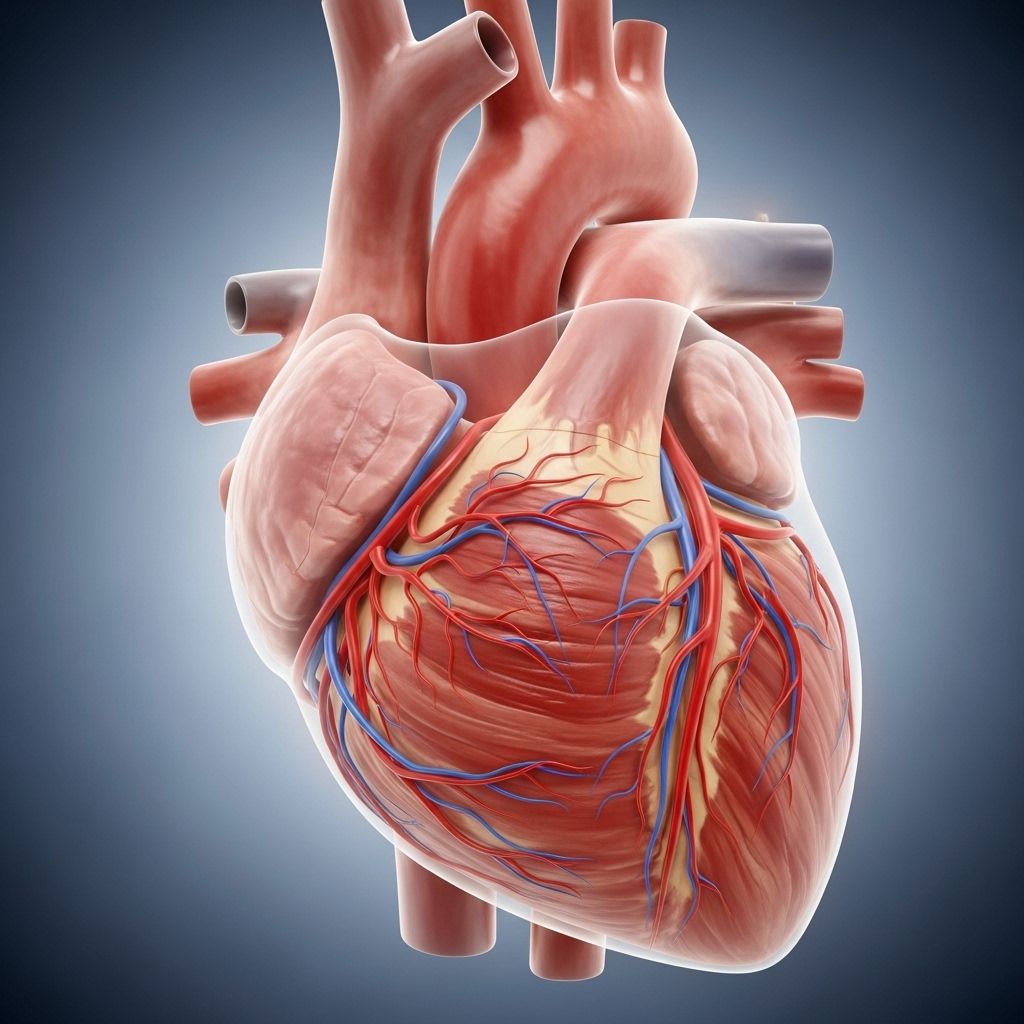
The heart, a muscular organ essential for life, relies on a continuous and regulated flow of oxygen-rich blood to function properly. This critical task is handled by the coronary arteries, a network of blood vessels that envelop and penetrate the heart muscle (myocardium). Understanding the anatomy and function of the coronary arteries is key to appreciating how the heart works and what can go wrong when these vessels are compromised.
Introduction: The Lifeline of the Heart
The coronary arteries are responsible for delivering oxygenated blood and vital nutrients directly to the heart muscle. Without this constant supply, the heart tissue can quickly become damaged or even die. This process is at the root of many cardiovascular diseases, including the most common, coronary artery disease (CAD).
- Coronary arteries arise from the base of the aorta and form a ring-like network around the heart.
- They branch into smaller vessels, supplying all regions of the myocardium.
- The heart depends entirely on these arteries for oxygen and nutrient delivery, as well as waste removal.
Coronary Arteries Overview
Coronary arteries are unique in that they must perform flawlessly throughout an individual’s life to ensure every heartbeat is met with adequate blood flow. There are two main coronary arteries:
- Right coronary artery (RCA)
- Left main coronary artery (LMCA)
Each main artery divides into several significant branches, forming an intricate and highly responsive system for perfusing the dynamic environment of the beating heart.
Key Facts About Coronary Arteries
- The coronary arteries supply approximately 250300 mL of blood per minute to the heart under resting conditions.
- They are subject to a variety of anatomical variations between individuals, influencing susceptibility to disease and response to interventions.
- Coronary arteries are classified by their location and the territory they supply: epicardial (on the heart’s surface) and microvascular (penetrating the myocardium).
Origins of the Coronary Arteries
Both the RCA and LMCA originate from the very beginning of the aorta, at areas called the aortic sinuses or the sinuses of Valsalva. These openings are located just above the aortic valve, a strategic position ensuring the freshest, most oxygen-rich blood is delivered directly to the heart muscle before any other body tissue.
- The right coronary artery arises from the right aortic sinus.
- The left main coronary artery emerges from the left aortic sinus.
This anatomical design ensures that the heart muscle receives blood during the diastolic phase of the cardiac cycle, when the myocardium is relaxed and the blood can flow inward.
The Two Main Coronary Arteries and Their Branches
| Artery | Major Branches | Supplied Territories |
|---|---|---|
| Left Main Coronary Artery (LMCA) |
|
|
| Right Coronary Artery (RCA) |
|
To distinguish between various heart conditions, it's vital to understand the differences between angina and coronary artery disease. By identifying symptoms and receiving timely diagnosis, you can significantly improve outcomes and maintain heart health. |
Left Main Coronary Artery (LMCA)
The left main coronary artery is relatively short but vital, quickly branching into arteries that supply the left side of the heart—the side responsible for pumping blood throughout the body.
- Left Anterior Descending (LAD) artery: Travels down the front (anterior) of the heart, supplying most of the front wall of the left ventricle and the anterior two-thirds of the interventricular septum. The LAD also gives off diagonal branches and septal perforators.
- Left Circumflex (LCx) artery: Loops around the left side of the heart, nourishing the outer and posterior surfaces of the left ventricle and left atrium via obtuse marginal branches.
- Ramus/intermediate artery (in some people): A third branch between the LAD and LCx, providing supplemental blood flow to adjacent territories.
Right Coronary Artery (RCA)
The right coronary artery courses along the right side of the heart and is responsible for perfusing the chambers on this side as well as the nodes that regulate cardiac rhythm:
- Right Marginal artery: Supplies the right ventricle.
- Posterior Descending Artery (PDA): Runs down the back of the heart in the posterior interventricular sulcus, supplying the lower part of the left and right ventricles and a portion of the interventricular septum.
The RCA is also the primary source of blood for the heart’s electrical conduction system via branches to the sinoatrial (SA) node and atrioventricular (AV) node in most people.
Other Coronary Artery Branches and Variations
The pattern of coronary artery branching and the areas they supply can vary from person to person. Notable variations include:
- The presence of a ramus/intermediate artery.
- A conus artery (in about 45% of the population) that may provide collateral circulation in certain cases.
- Posterior Descending Artery (PDA) can arise from either the RCA (most common, called right-dominant), the left coronary via the circumflex (left-dominant), or both (co-dominant).
Microvascular and Epicardial Arteries
Coronary arteries can be further described based on their location:
- Epicardial arteries: Major coronary arteries that lie on the outer surface of the heart. These arteries are commonly affected by atherosclerosis and thereby coronary artery disease.
- Microvascular arteries: Smaller vessels that penetrate the heart muscle and supply deeper myocardial tissue. These may become functionally impaired in microvascular angina.
Functional Anatomy and Blood Flow
The heart is unique in that coronary blood flow occurs predominantly during the relaxation phase of the heartbeat (diastole). During contraction (systole), the heart muscle compresses these vessels, especially the smaller intramural arteries, reducing blood flow.
- During diastole: Blood flows freely through the coronary circulation, entering myocardial capillaries where oxygen and nutrients are exchanged for carbon dioxide and metabolic waste.
- During systole: The intramural branches are compressed, momentarily reducing flow, particularly in the left ventricle.
Coronary Circulation and Venous Return
After oxygen delivery, deoxygenated blood is collected by the coronary veins and returns to the right atrium through the coronary sinus, completing the cardiac circulation loop.
Clinical Importance of the Coronary Arteries
Any compromise to the function of the coronary arteries can have profound effects on the health of the heart and the entire body. Major clinical conditions related to these arteries include:
- Coronary artery disease (CAD): Narrowing or blockage of the epicardial arteries, usually due to atherosclerosis, which can cause angina (chest pain) or myocardial infarction (heart attack).
- Spasm or microvascular dysfunction: Can cause reduced blood supply (ischemia), even with clear large arteries.
- Anomalies of origin or course: Rare variations in how coronaries arise or branch can affect risk of sudden cardiac death, especially in young athletes.
Risk Factors for Coronary Artery Disease
- High cholesterol levels
- High blood pressure (hypertension)
- Smoking
- Diabetes
- Family history of heart disease
- Obesity and lack of physical activity
Maintaining healthy coronary arteries is a crucial aspect of preventing cardiovascular events.
Diagnostic Tools for Coronary Artery Assessment
Modern medicine offers a variety of tests to study coronary arteries and diagnose problems:
- Coronary angiography: A special dye and x-ray technique that visualizes the inside of coronary arteries for blockages.
- Computed Tomography Coronary Angiography (CTCA): Provides detailed 3D images of the coronary vessels.
- Magnetic Resonance Angiography (MRA): An MRI-based approach for vessel mapping.
- Stress testing: Monitors the heart’s response to exertion, which can uncover reduced blood flow from narrowing arteries.
Treatments and Prevention of Coronary Artery Disease
Efforts to manage and prevent coronary artery disease focus equally on lifestyle, medications, and advanced interventions:
- Lifestyle modification: Diet, exercise, smoking cessation, and weight management.
- Medications: Statins, antiplatelet drugs, beta-blockers, ACE inhibitors, and nitrates as indicated.
- Interventional procedures: Angioplasty and stent placement can open blocked arteries.
- Coronary artery bypass grafting (CABG): Surgical creation of alternate pathways using vessels from other parts of the body.
Key Points to Remember
- The coronary arteries are the exclusive suppliers of blood to the heart muscle.
- There are two main arteries (RCA and LMCA), both with critical branches.
- Damage or narrowing of these vessels can severely compromise heart function.
- Early diagnosis and preventive measures are vital in maintaining coronary and overall heart health.
Frequently Asked Questions (FAQs)
Q: What are the coronary arteries?
A: The coronary arteries are specialized blood vessels that deliver oxygen-rich blood to the heart muscle, ensuring its survival and optimal function.
Q: What happens when the coronary arteries become narrowed or blocked?
A: Narrowing or blockage—often due to atherosclerosis (buildup of plaque)—can reduce oxygen supply, causing chest pain (angina) or myocardial infarction (heart attack).
Q: Why are the left anterior descending (LAD) and right coronary arteries so clinically significant?
A: These arteries supply large and essential regions of the heart. Blockage of the LAD, sometimes called the “widow-maker,” is often life-threatening because it cuts off blood to the front wall of the left ventricle, a critical pump chamber.
Q: Can coronary artery anatomy vary among different people?
A: Yes, anatomical variations are common; some people may have extra branches, a different origin of arteries, or differences in dominance (which artery gives rise to the PDA).
Q: How can I keep my coronary arteries healthy?
A: Follow a healthy lifestyle—don’t smoke, eat a balanced diet, exercise regularly, manage blood pressure and cholesterol, and maintain a healthy weight. Regular checkups and early intervention for risk factors are also essential.
References
Read full bio of Sneha Tete












