AML vs. ALL: Key Differences in Types, Symptoms, and Treatments
Explore the crucial distinctions between acute myeloid leukemia (AML) and acute lymphocytic leukemia (ALL), from diagnosis to outcomes.
Acute Myeloid Leukemia (AML) vs. Acute Lymphocytic Leukemia (ALL): What Sets Them Apart?
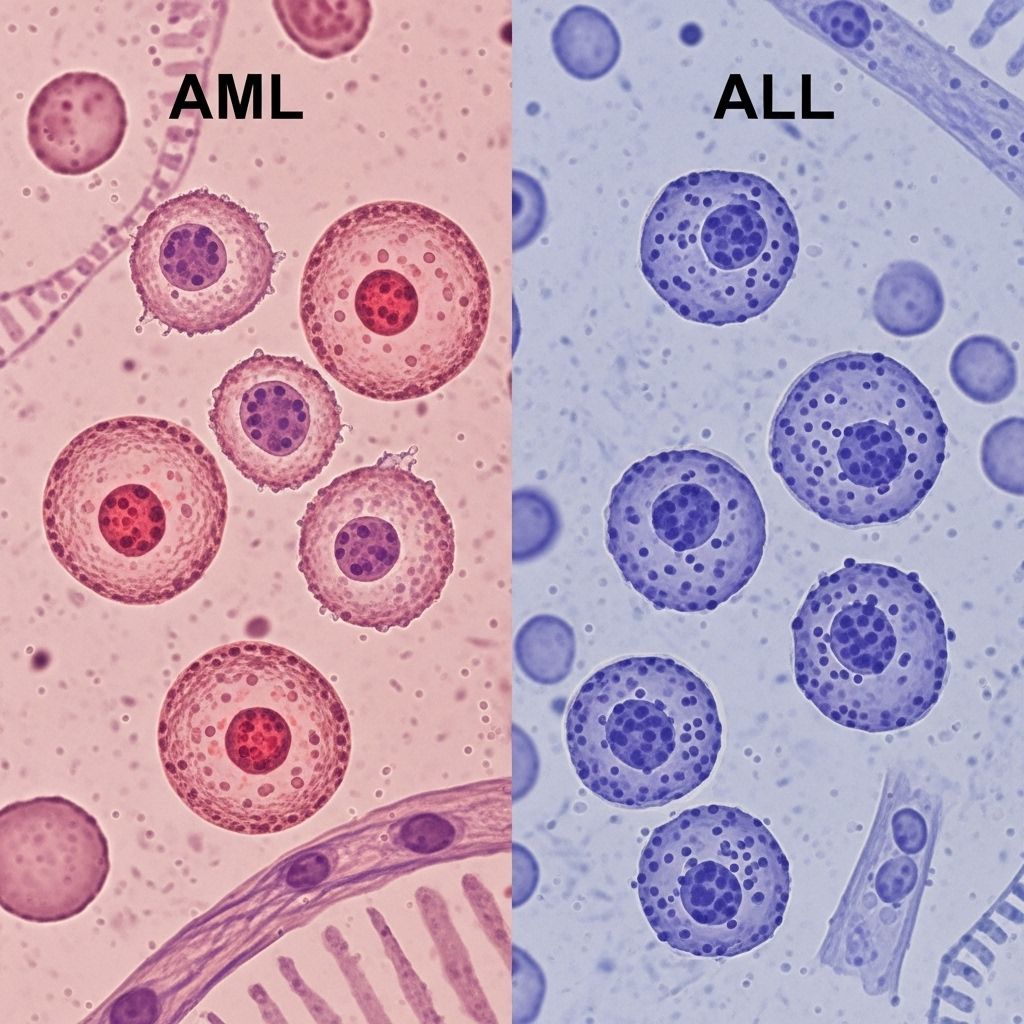
Leukemia describes a group of cancers that affect the blood and bone marrow, disrupting the body’s ability to generate normal blood cells. Among the most aggressive forms are acute myeloid leukemia (AML) and acute lymphocytic leukemia (ALL). Although these two leukemias can appear similar, they arise from different cell types and have distinct effects, symptoms, diagnostic processes, and treatment strategies.
Understanding AML and ALL
To appreciate the differences between AML and ALL, it’s essential to first understand the role of blood cells and how their development goes awry in these cancers.
- AML originates from myeloid precursor cells. These cells normally mature into various blood components, such as granulocytes (types of white blood cells that fight infection), monocytes, red blood cells, and platelets.
- ALL develops from lymphoid precursor cells, which typically become lymphocytes—mainly T cells, B cells, or natural killer (NK) cells. These cells are primarily responsible for immune defense.
While AML is more commonly diagnosed in adults, especially older adults, ALL is the most common type of leukemia found in children, though it can also affect adults.
| Feature | AML | ALL |
|---|---|---|
| Cell of origin | Myeloid precursor cell | Lymphoid precursor cell |
| Age group most affected | Adults (especially older adults) | Children (but also adults) |
| Prevalence | Most common acute leukemia in adults | Most common leukemia in children |
| Normal cell types lost | Red blood cells, platelets, granulocytes | B cells, T cells, NK cells |
Symptom Comparison
The symptoms of AML and ALL are generally due to a decline in healthy blood cell production, leading to similar manifestations. However, certain symptoms can provide clues as to which type of leukemia may be present.
| Symptom | AML | ALL |
|---|---|---|
| Abdominal swelling | ✔️ | ✔️ |
| Bleeding gums | ✔️ | ✔️ |
| Bone pain | ✔️ | ✔️ |
| Fatigue, weakness, pale skin | ✔️ | ✔️ |
| Dizziness or lightheadedness | ✔️ | ✔️ |
| Easy bruising, frequent nosebleeds, excessive bleeding | ✔️ | ✔️ |
| Enlarged lymph nodes | ✔️ | ✔️ (more common/severe) |
| Enlarged spleen or liver | ✔️ (potentially) | ✔️ |
| Heavy menstrual periods | ✔️ | ✔️ |
| Loss of appetite, weight loss | ✔️ | ✔️ |
| Frequent infections | ✔️ | ✔️ |
| Night sweats | ✔️ | ✔️ |
| Swollen thymus, changes in awareness | Rare | ✔️ (unique to ALL) |
| Headaches | Rare | ✔️ |
| Joint pain | ✔️ | ✔️ |
- Symptoms such as abdominal swelling, bone pain, bleeding, bruising, fever, and shortness of breath can appear in both types.
- ALL may involve swelling of the thymus, which can compress airways and blood vessels, resulting in headaches, dizziness, facial swelling, or changes in awareness—these are rare in AML.
- Both AML and ALL sufferers are at higher risk of infections due to low white blood cell counts.
Risk Factors
While both conditions can arise seemingly without cause, certain factors are known or suspected to increase risk:
- AML:
- Exposure to radiation or certain chemicals (such as benzene)
- Previous chemotherapy or radiation for other cancers
- Smoking
- Genetic syndromes like Down syndrome
- Aging: risk increases with age, especially after 60
Recognizing the unique risk factors for Acute Lymphoblastic Leukemia (ALL) is vital for prevention and early action. To empower your understanding, explore our insightful article on childhood Acute Lymphoblastic Leukemia and its associated risks. - ALL:
- Genetic factors (including Down syndrome and other inherited syndromes)
- Exposure to certain chemicals or radiation
- Having a sibling with ALL
- Most common in children, but can occur at any age
Diagnosis
Diagnosing AML and ALL requires a combination of clinical evaluation, laboratory tests, and sometimes genetic analysis.
- Blood tests: Most cases are first indicated by abnormal findings in a complete blood count (CBC), such as too many white blood cells (blasts), low red blood cells, or low platelets.
- Bone marrow biopsy: A sample of bone marrow reveals the predominant type of abnormal cell—myeloblasts in AML, lymphoblasts in ALL.
- Other tests: Additional lab tests may assess organ function, identify any infections, or check for specific genetic mutations or chromosome changes that can help refine the diagnosis and guide treatment.
- Imaging: Scans might be used to evaluate organ involvement, such as an enlarged spleen or lymph nodes, or to check for a mass in the mediastinum (seen in ALL when the thymus is affected).
Treatments
AML and ALL are both treated intensively, often using a combination of chemotherapy, targeted drugs, supportive care, and in some cases, stem cell transplantation. The exact regimen depends on age, overall health, and the genetic makeup of the leukemia cells.
Standard AML Treatments
- Induction chemotherapy: Often the first step, aiming to achieve remission by killing leukemia blasts in the bone marrow. Common drugs include cytarabine and anthracyclines.
- Consolidation (post-remission) therapy: Further chemotherapy to eliminate any remaining leukemia cells and lower the risk of relapse.
- Targeted therapies: For cases with certain mutations (like FLT3), drugs may specifically target the abnormal leukemia cells.
- Bone marrow or stem cell transplantation: May be considered for younger or higher-risk patients, especially if remission is achieved but relapse risk remains high.
- Supportive care: Transfusions, antibiotics, and treatments to boost blood cell counts or decrease infection risk.
Standard ALL Treatments
- Induction therapy: Intensive chemotherapy often using a combination of drugs (such as vincristine, dexamethasone, anthracyclines, and asparaginase) to bring about remission.
- CNS prophylaxis: Because ALL can spread to the brain and spinal cord, preventive (prophylactic) therapies—like lumbar punctures with chemotherapy or cranial irradiation—are used.
- Consolidation and maintenance therapy: After remission, further chemotherapy—and sometimes oral drugs—are administered for several months to years to prevent relapse.
- Targeted therapies or immunotherapy: Some people may receive drugs that target specific leukemia cell mutations or harness the body’s immune system to fight leukemia (e.g., CAR-T cell therapy).
- Stem cell transplantation: Used for certain high-risk patients or those not responding fully to other treatments.
Outlook and Survival
Survival rates for AML and ALL have improved significantly, especially for certain age groups, but there are notable differences between the two.
- AML: Five-year survival for adults is about 30%, but this varies greatly by age, underlying health, and genetic features of the leukemia. Younger or healthier patients tend to fare better.
- ALL: Five-year survival is much higher in children (as high as 90%), but outcomes are less favorable in adults, where survival rates are closer to 40%.
- Certain genetic changes in leukemia cells may make the disease more or less responsive to therapy, affecting the outlook.
- Relapse is possible for both AML and ALL, requiring further treatment or a change in therapy strategy.
A Note About Hope
While a diagnosis of AML or ALL can be overwhelming, advancements in treatment have opened many new options. Clinical trials continue to drive research forward, exploring innovative therapies such as targeted drugs, novel chemotherapies, and immune-based treatments. Support networks, including counseling and peer groups, are vital resources to help patients and families navigate their journey.
Frequently Asked Questions (FAQs) About AML and ALL
What is the main difference between AML and ALL?
AML affects myeloid cells, which give rise to most white blood cells, red blood cells, and platelets. ALL affects lymphoid cells, a type of white blood cell responsible for immune responses.
Which type of leukemia is more common in children?
ALL is more common in children, representing the majority of pediatric leukemia cases.
Are the treatments for AML and ALL the same?
No. Although both may use chemotherapy and transplantation, drug choices, regimens, and the approach to central nervous system involvement differ substantially.
What are some warning signs that should prompt a doctor’s visit?
Persistent fatigue, unexplained fever, frequent infections, easy bruising or bleeding, swollen lymph nodes, or excessive night sweats warrant medical evaluation, especially if they persist or worsen.
Is a cure possible for AML or ALL?
Many children with ALL can be cured, and some adults with AML can achieve long-term remission or cure. Outcomes continue to improve as newer therapies become available.
Key Takeaways
- AML and ALL are two forms of acute leukemia with important biological and clinical distinctions.
- Both require prompt and specialized treatment, but their recovery rates and strategies differ.
- Awareness of the symptoms and risk factors can help with earlier detection and improved outcomes.
- Continuous advancements in research give hope for further improvements in survival and quality of life for patients diagnosed with these conditions.
References
- https://www.patientpower.info/leukemia/aml-vs-all
- https://www.healthline.com/health/leukemia/aml-vs-all
- https://www.medicalnewstoday.com/articles/aml-vs-all
- https://www.cancercenter.com/community/blog/2024/03/aml-vs-all
- https://www.webmd.com/cancer/lymphoma/leukemia-all-vs-aml
- https://www.ncbi.nlm.nih.gov/books/NBK560490/
- https://www.mdanderson.org/cancer-types/leukemia.html
- https://www.myleukemiateam.com/resources/acute-lymphoblastic-leukemia-vs-acute-myeloid-leukemia-understanding-the-difference
- https://www.youtube.com/watch?v=Uyp6WLVsnys
Read full bio of medha deb












