ALK Positive Lung Cancer: Essential Facts and Updated Insights
An in-depth look at ALK positive lung cancer’s unique nature, diagnosis, treatment options, and outlook for patients.
ALK Positive Lung Cancer: What to Know
Lung cancer remains one of the most diagnosed and researched cancers worldwide, but recent advances have clarified that it is not a single disease. Among its many forms is ALK positive lung cancer—a unique subset that responds especially well to certain targeted therapies. Understanding this type’s genetics, symptoms, prognosis, and modern treatments can significantly influence care and outcomes.
Table of Contents
- What is ALK Positive Lung Cancer?
- How Common is ALK Positive Lung Cancer?
- Symptoms of ALK Positive Lung Cancer
- Causes and Risk Factors
- Diagnosis and Testing for ALK Mutations
- Stages of ALK Positive Lung Cancer
- Treatment Options
- Life Expectancy and Survival Rates
- Is ALK Positive Lung Cancer Hereditary?
- Frequently Asked Questions (FAQs)
What is ALK Positive Lung Cancer?
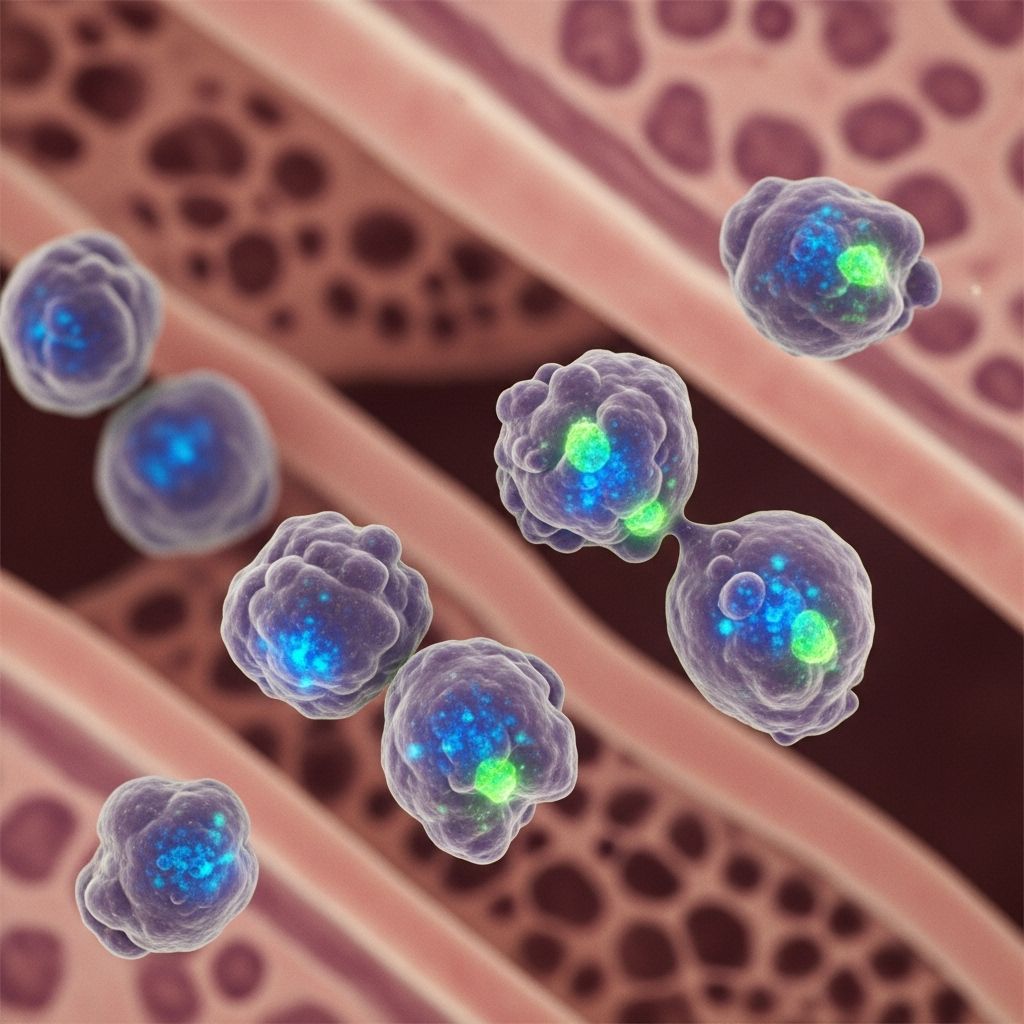
ALK stands for anaplastic lymphoma kinase—a gene present in all humans. In ALK positive lung cancer, a specific mutation causes an abnormal gene fusion event, typically between the EML4 and ALK genes. This fusion produces a mutant protein that triggers uncontrolled cell division and cancer growth.
Most commonly, ALK mutations are seen in non-small cell lung cancer (NSCLC), especially in the adenocarcinoma subtype. These alterations cause the affected lung cells to multiply rapidly, forming tumors and sometimes spreading throughout the body.
This condition was first widely recognized in 2007 and represents an important area of lung cancer research and treatment, particularly because it allows for targeted therapies that greatly improve outcomes for patients compared to older treatment strategies.
How Common is ALK Positive Lung Cancer?
ALK positive lung cancers are relatively rare but significant in the landscape of lung cancer:
- Around 5% of people with non-small cell lung cancer have ALK positive mutations, according to global cancer statistics.
- This subtype corresponds to approximately 72,000 diagnoses worldwide each year.
- It predominantly affects younger patients, often females, who are under age 50 and have never smoked.
This makes ALK positive lung cancer distinct among typical lung cancer cases, which are more commonly found in older individuals and those with a history of smoking.
Symptoms of ALK Positive Lung Cancer
The symptoms of ALK positive lung cancer are similar to those of other non-small cell lung cancers and may not appear until the disease has progressed. Common symptoms include:
- Persistent cough that does not go away
- Chest pain, often worsening with deep breaths, laughing, or coughing
- Shortness of breath
- Hoarseness of the voice
- Wheezing
- Coughing up blood (hemoptysis)
- Loss of appetite
- Unexplained weight loss
- General weakness or fatigue
Because these symptoms can mimic less serious conditions like respiratory infections, ALK positive lung cancer can sometimes be missed—especially in younger, non-smoking patients. Early and proactive testing is essential if these symptoms persist without clear explanation.
Causes and Risk Factors
The ALK mutation is not fully understood, but current knowledge offers several key insights:
- Gene fusions involving ALK do not run in families and are not heritable.
- The mutation typically arises spontaneously during a person’s lifetime; the exact triggers for this fusion event remain unknown.
- Unlike many other lung cancer types, there is no clear link with smoking, environmental exposures, or familial risk.
- It most frequently affects younger individuals (often under the age of 50), and tends to occur more in women.
Researchers continue to investigate why this mutation appears in certain people. Meanwhile, established risk factors for general lung cancer, such as tobacco use, have little bearing on the risk for ALK positive NSCLC.
Diagnosis and Testing for ALK Mutations
In cases where lung cancer is suspected, accurate diagnosis and determination of ALK status are crucial steps:
- Tissue Biopsy: A sample of cancer cells is taken via bronchoscopy, needle biopsy, or surgery. This tissue is analyzed for ALK gene changes.
- Biomarker Testing: Tumor cells are tested for various genetic mutations such as ALK, ROS1, or EGFR using advanced laboratory techniques like fluorescence in situ hybridization (FISH), immunohistochemistry (IHC), or next-generation sequencing (NGS).
- Liquid Biopsy: In some cases, blood samples may reveal circulating tumor DNA carrying the ALK fusion.
Identifying these specific genetic alterations informs the treatment plan by directing doctors toward targeted therapies that can yield better results than traditional chemotherapy alone.
Stages of ALK Positive Lung Cancer
The prognosis and treatment of ALK positive lung cancer depend heavily on the stage at which it is diagnosed. Staging describes how much the tumor has grown and if it has spread beyond the lungs.
| Stage | Description |
|---|---|
| Stage 0 | Cancer cells found only in the top airway lining; no deeper lung or lymph node involvement. |
| Stage 1A | Tumor is 1–3 cm in diameter, confined within the lung. |
| Stage 1B | Tumor is 3–4 cm, may affect deeper lung tissues. |
| Stage 2A | Tumor is 4–5 cm, and possibly involves deeper tissues. |
| Stage 2B | Tumor size 4–5 cm, may affect lymph nodes. |
| Stage 3A | Tumor is 5–7 cm; cancer has spread within the lung. |
| Stage 3B | Cancer starts to affect the chest wall or areas around the heart. |
| Stage 4 | Cancer spreads to the other lung and distant organs (liver, brain, etc.). |
Early-stage cancers are often found incidentally during scans for other reasons, as symptoms tend to appear only after significant growth or metastatic spread.
Treatment Options
The recognition of ALK mutations in lung cancer has revolutionized therapy with the use of ALK inhibitors—targeted drugs that block the faulty protein driving tumor growth. Treatment can vary depending on the cancer’s stage and patient health:
- Targeted Therapy: Frontline treatment for ALK positive NSCLC. Drugs such as crizotinib, ceritinib, alectinib, brigatinib, and lorlatinib have all been approved for ALK positive lung cancer and offer higher response rates, longer disease control, and less toxicity compared to traditional treatments.
- Chemotherapy: Older but occasionally still used, especially if targeted therapy stops working or is not well-tolerated.
- Immunotherapy and Other Drugs: Not typically as effective in ALK positive lung cancer compared to other forms, but might be considered in certain settings or as part of combination therapy.
- Surgery: May be considered when the disease is detected at an early stage and localized.
- Radiation Therapy: Used in select cases, especially for tumors that cannot be removed surgically or when cancer has spread to specific regions like the brain.
Continuous research means that new drugs and combinations are regularly being studied to overcome the cancer’s ability to develop drug resistance over time.
Life Expectancy and Survival Rates
The introduction of targeted therapies has dramatically improved the prognosis for ALK positive lung cancer compared with historical figures for lung cancer generally.
- Before ALK inhibitors, the average survival for metastatic ALK positive lung cancer often ranged from 6–12 months.
- With modern ALK inhibitors, median survival times can exceed 5 years for many individuals, and ongoing innovations may yield even better results.
- Outcomes vary based on stage at diagnosis, overall health, response to treatment, and the development of resistance.
Regular monitoring and the availability of second- and third-generation ALK inhibitors make it possible for many patients to maintain good quality of life and longer survival.
Is ALK Positive Lung Cancer Hereditary?
Unlike certain breast or colon cancers tied to inherited mutations, the ALK fusion is a somatic (acquired) mutation that does not get passed from parents to children.
- There is no hereditary pattern observed with ALK positive lung cancer.
- Family members of patients with ALK positive NSCLC do not have an increased risk of developing the same malignancy as a result of heredity.
- This mutation arises during a person’s life, typically due to spontaneous inaccuracies during the process of cell replication.
Frequently Asked Questions (FAQs)
What is the outlook for people diagnosed with ALK positive lung cancer?
Thanks to effective targeted therapies, many people with ALK positive NSCLC experience years of good disease control with manageable side effects compared to standard therapies. Median survival times with current treatments often range between 4 to 7 years, and some patients live longer with new therapies in development.
Who should be tested for ALK positive lung cancer?
All individuals diagnosed with non-small cell lung cancer, especially the adenocarcinoma subtype, should have their tumors tested for ALK and other biomarkers to guide therapy. Young, non-smoking lung cancer patients are particularly likely to have actionable mutations, but testing is recommended for all regardless of demographic or smoking history.
Are ALK inhibitors safe, and what are their side effects?
ALK inhibitors are generally well-tolerated compared to traditional chemotherapy, but side effects can occur. Common reactions include nausea, fatigue, diarrhea, swelling, vision changes, and liver enzyme elevations. Most side effects are manageable, and drug development aims to further reduce toxicity while maintaining effectiveness.
Can ALK positive lung cancer be cured?
A true cure is rare, especially when the disease is already advanced at diagnosis, but many patients can maintain long-term disease control. Early-stage cancers treated with surgery and follow-up therapies have a higher chance of long-term remission.
Is smoking linked to ALK positive lung cancer?
No. Most people diagnosed with ALK positive lung cancer are non-smokers or have only minimal exposure. Smoking is not considered a primary risk factor for this mutation.
Takeaway
ALK positive lung cancer is a unique and increasingly treatable subtype of non-small cell lung cancer. While not common, it represents an important category where genetic testing and personalized therapy have revolutionized outcomes. Advances in targeted drugs, vigilant biomarker testing, and growing knowledge about the genetic causes mean that people with ALK positive lung cancer have more hope and options than ever before. Ongoing research promises new breakthroughs and continued improvements in care and survival for this group of patients.
References
- https://www.healthline.com/health/lung-cancer/alk-postive-lung-cancer-what-to-know
- https://alkpositive.org/what-is-alk/
- https://www.medicalnewstoday.com/articles/alk-non-small-cell-lung-cancer
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/symptoms-diagnosis/biomarker-testing/alk-lung-cancer
- https://www.healthline.com/health/nsclc/guide-to-lung-cancer-mutations
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9989809/
- https://alk.lungevity.org/alk/about-alk-positive-lung-cancer
- https://lcfamerica.org/about-lung-cancer/diagnosis/biomarkers/alk/
Read full bio of medha deb












