Alcohol-Induced Liver Disease: Causes, Symptoms, Diagnosis, and Treatment
Comprehensive guide to alcohol-induced liver disease, covering risk factors, symptoms, stages, diagnosis, and treatment strategies.
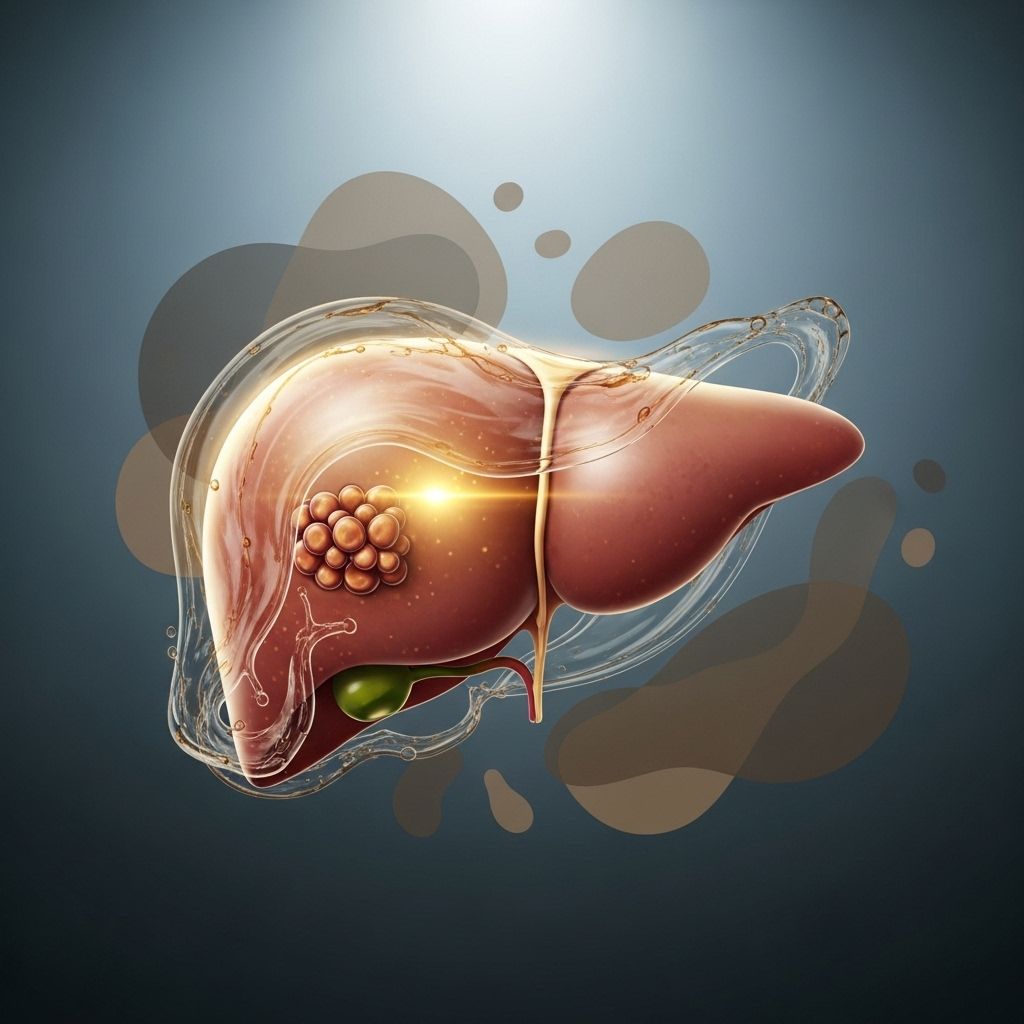
Alcohol-Induced Liver Disease
Alcohol-induced liver disease is a serious medical condition resulting from prolonged and excessive alcohol consumption, which damages the liver and impairs its ability to perform vital functions. This condition encompasses a spectrum of liver damage, ranging from simple fatty liver to cirrhosis—a potentially fatal form of liver scarring and liver failure.
Understanding the Liver’s Role in Alcohol Metabolism
The liver is the body’s primary organ for processing and detoxifying substances such as alcohol. About 98 percent of consumed alcohol is metabolized by the liver. Persistent heavy drinking can overwhelm the liver’s detoxification mechanisms, leading to accumulation of fats, inflammation, and eventual scarring. Interestingly, recent research indicates that other organs such as the intestines and fat tissues can partially compensate for hindered liver alcohol metabolism, though they do not prevent the progression of liver damage.
- Fatty liver (steatosis): Earliest and most common form; excess fat accumulates in liver cells.
- Alcoholic hepatitis: Inflammation and damage of liver cells, potentially reversible with abstinence.
- Cirrhosis: Irreversible scarring that impairs liver function, leading to life-threatening complications.
Causes and Risk Factors
Alcohol-induced liver disease stems primarily from chronic and heavy alcohol intake. Not everyone who drinks heavily will develop liver disease, but the risk increases with:
- Duration and quantity of alcohol consumption
- Genetic predisposition affecting alcohol metabolism
- Gender (female biological sex): Women have a higher susceptibility at lower doses
- Co-existing chronic infections (e.g., hepatitis B or C)
- Poor nutrition or obesity
- Other health conditions such as diabetes
Symptoms of Alcohol-Induced Liver Disease
Many people may not exhibit noticeable symptoms in the early stages. As liver disease progresses, signs become more pronounced:
- Fatigue
- Loss of appetite
- Weight loss
- Nausea or vomiting
- Abdominal pain or tenderness (especially in upper right side)
- Jaundice (yellowing of skin and eyes)
- Swelling in legs and abdomen
- Easy bruising or bleeding
- Confusion, difficulty concentrating (hepatic encephalopathy)
Stages of Alcohol-Induced Liver Disease
| Stage | Description | Reversibility |
|---|---|---|
| Alcoholic Fatty Liver Disease | Excess accumulation of fat in the liver cells. Often asymptomatic. | Yes, with complete abstinence |
| Alcoholic Hepatitis | Inflammation and injury to liver cells; can be mild or severe. | Partially; mild cases may recover with abstinence |
| Cirrhosis | Permanent scarring of the liver, severely affecting its function. | No; progression can only be slowed |
Diagnosis
Diagnosis of alcohol-induced liver disease typically involves:
- Medical history and physical examination
- Blood tests: Elevated liver enzymes (ALT, AST), bilirubin, and decreased albumin
- Imaging studies: Ultrasound, CT scan, or MRI to assess liver size, texture, and presence of fat or scar tissue
- Liver biopsy: In select cases, a small tissue sample confirms the type and extent of liver injury
Doctors may also assess for complications such as portal hypertension (increased pressure in the blood vessels of the liver), ascites (fluid accumulation), and signs of liver failure.
Complications
- Portal Hypertension: Increased pressure within the portal vein, leading to swollen veins (varices), especially in the esophagus.
- Ascites: Fluid buildup in the abdomen due to impaired protein synthesis by the liver.
- Hepatic Encephalopathy: Toxin buildup affects brain function, leading to confusion and potential coma.
- Increased bleeding risk: Liver’s reduced ability to produce clotting factors.
- Liver cancer (hepatocellular carcinoma): Higher risk due to chronic inflammation and scarring.
Treatment Options
The cornerstone of treatment for alcohol-induced liver disease is complete abstinence from alcohol. Damage to the liver can be partially reversed if detected early and alcohol is stopped altogether. Specific treatment strategies may include:
- Alcohol cessation programs: Medical detox, counseling, and support groups
- Nutritional support: High-calorie, protein-rich diets to prevent muscle wasting
- Medications: Corticosteroids for severe alcoholic hepatitis, though only a subset of patients respond positively.
Other drugs to manage specific complications (e.g., diuretics for ascites, beta-blockers for portal hypertension) - Management of complications: Treating infections, preventing bleeding, addressing hepatic encephalopathy
- Liver transplantation: Reserved for advanced disease when medical therapy is unsuccessful and strict criteria are met
Potential New Treatments
- Polyunsaturated lecithin supplements: In animal studies, lecithin prevented progression of early liver fibrosis, but more research is needed before human application
- Targeted therapies: Ongoing research into inflammation pathways and immune response modulation
Liver Transplantation
For patients with end-stage liver disease, liver transplantation offers a chance at survival, but availability is limited and strict criteria must be met. Historically, a six-month period of abstinence was required before consideration for transplant. However, recent studies challenge this rule, showing that early transplantation in critically ill patients greatly improves survival rates:
- Survival rates: Approximately 89-100% survival after six months and one year, compared to 11% without transplantation*
- Relapse risk: Slightly higher risk for alcohol relapse in early transplant recipients, but overall outcomes are favorable with careful patient selection
Selection criteria exclude patients with active severe psychiatric illness, insufficient social support, or ongoing substance abuse. The multidisciplinary team assesses psychological readiness and ability to maintain sobriety post-transplant.
Post-Transplant Care
- Ongoing addiction therapy and counseling
- Immunosuppressive management to prevent organ rejection
- Regular follow-up evaluations
Prevention Strategies
Prevention of alcohol-induced liver disease centers on minimizing alcohol intake and promoting overall liver health. Helpful strategies include:
- Limiting alcohol consumption to safe levels as recommended by health authorities
- Seeking help for alcohol use disorder (AUD) early
- Regular screening for liver enzyme elevations in high-risk individuals
- Maintaining a balanced diet rich in antioxidants and essential nutrients
- Vaccination against hepatitis viruses where appropriate
Living with Alcohol-Induced Liver Disease
Managing this condition requires lifelong commitment to lifestyle changes and regular medical follow-up. Tips for living with liver disease:
- Never resume drinking alcohol once diagnosed
- Maintain a healthy weight and exercise regularly
- Follow dietary recommendations and avoid hepatotoxic medications
- Engage in regular mental health support and counseling
- Stay vigilant for symptoms indicative of disease progression
Frequently Asked Questions (FAQs)
Q: Can liver damage from alcohol be reversed?
A: Fatty liver changes can be reversed with complete abstinence. Mild alcoholic hepatitis may also recover, but cirrhosis is irreversible; progression can be slowed with sobriety and proper medical care.
Q: What is the outlook for patients with alcoholic liver disease?
A: Prognosis depends on the stage at diagnosis. Early detection and abstinence improve outcomes. Advanced disease carries higher risk of death, unless liver transplantation is an option.
Q: Are women more at risk for alcohol-induced liver disease?
A: Yes; women are more likely to develop liver damage at lower levels of alcohol intake due to differences in body composition and metabolism.
Q: How is alcoholic hepatitis treated?
A: Treatment is mainly supportive—alcohol cessation, nutrition, and sometimes corticosteroid therapy for severe cases. Liver transplantation is considered for patients not responding to medical therapy.
Q: Who qualifies for a liver transplant due to alcohol-related liver damage?
A: Qualification requires medical assessment, abstinence, psychosocial evaluation, and demonstration of readiness to maintain sobriety and follow complex care regimens.
Key Takeaways
- Alcohol-induced liver disease is preventable and treatable in early stages
- Complete abstinence is the most effective intervention
- Early diagnosis and ongoing medical support improve chances for stable health
- Liver transplantation is an evolving option for advanced cases with careful selection
- Prevention and education are crucial to reduce the burden of disease in populations
References
- https://irp.nih.gov/blog/post/2024/04/double-trouble-for-alcohol-associated-liver-disease
- https://www.youtube.com/watch?v=_7sAhQQmyX0
- https://www.youtube.com/watch?v=S8BCExUiu6w
- https://pure.johnshopkins.edu/en/publications/treatment-of-alcoholic-liver-disease-4
- https://pure.johnshopkins.edu/en/publications/early-liver-transplantation-in-acute-alcoholic-hepatitis
- https://www.broadcastmed.com/gastroenterology/5225/news/johns-hopkins-among-few-in-u-s-to-offer-early-liver-transplants-for-patients-with-alcohol-associated-liver-disease
Read full bio of medha deb












