Age-Related Macular Degeneration (AMD): Causes, Symptoms, Diagnosis, and Treatment
A comprehensive guide to age-related macular degeneration: causes, types, risk factors, diagnosis, management, and living with AMD.
Age-related macular degeneration (AMD) is a progressive eye disease—most often affecting individuals over 50 years old—that results in the deterioration of the macula, the central part of the retina responsible for sharp, straight-ahead vision. AMD is a leading cause of vision loss in older adults, though it does not cause complete blindness, as peripheral vision typically remains intact. Early detection, understanding risk factors, and innovative treatments can help manage and slow the progression of the disease.
What Is Age-Related Macular Degeneration (AMD)?
AMD is characterized by the gradual deterioration of cells in the macula—a small but critical area of the retina. The macula controls your central vision, which is essential for tasks requiring fine detail such as reading, recognizing faces, and driving. AMD primarily affects older adults, though various factors can increase susceptibility.
While AMD does not lead to total blindness, the loss of central vision can significantly impact daily activities and reduce quality of life. Importantly, the disease often progresses without early symptoms, making regular eye examinations crucial for detection and intervention.
Types of Age-Related Macular Degeneration
There are two primary types of AMD, each with unique features and progression patterns:
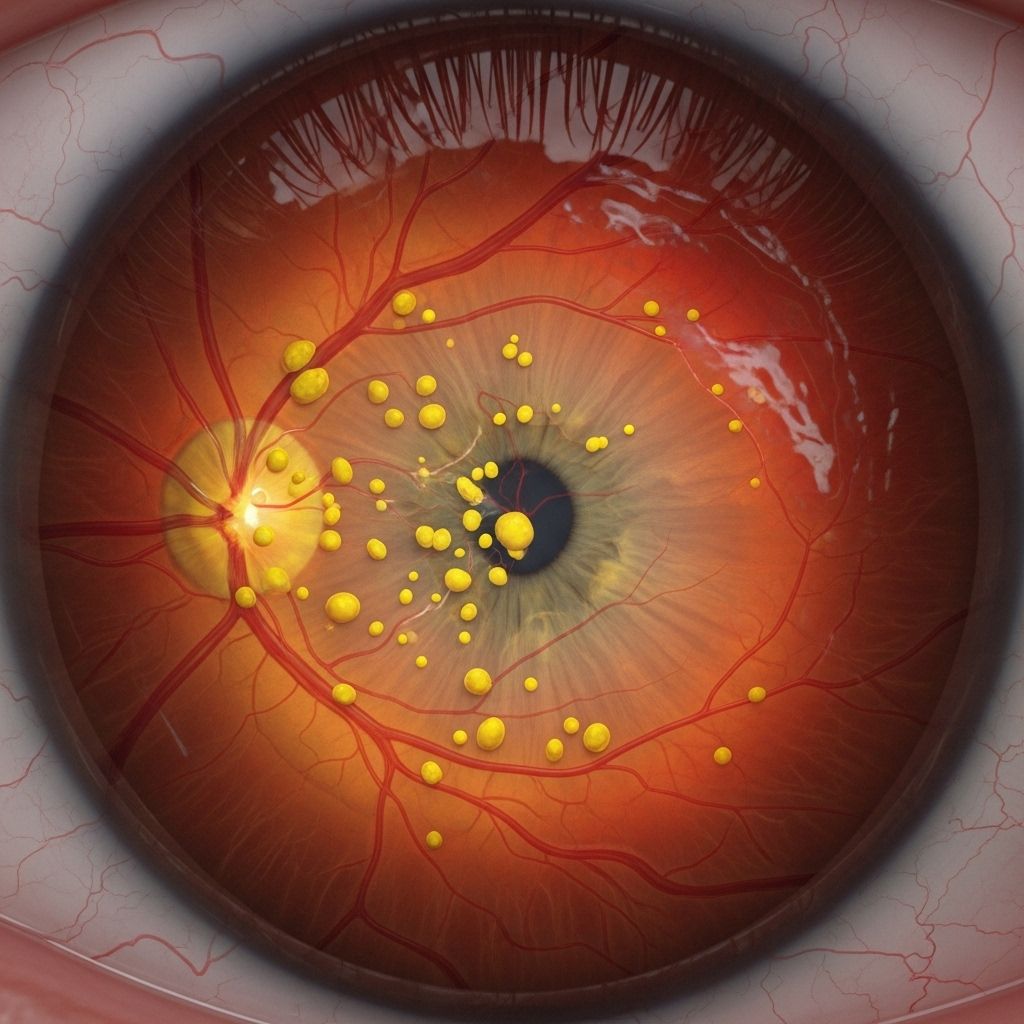
- Dry AMD (Atrophic AMD): The more common form, accounting for about 80–90% of AMD cases. Dry AMD advances slowly as light-sensitive cells in the macula break down and drusen (tiny yellow deposits) accumulate underneath the retina.
- Wet AMD (Neovascular or Exudative AMD): Though less common (10–20% of AMD cases), wet AMD is more severe and progresses rapidly. It occurs when abnormal blood vessels grow beneath the retina and leak blood or fluid, causing scarring and rapid vision distortion or loss.
Stages of Dry AMD
- Early Dry AMD: Characterized by small drusen and usually no noticeable symptoms.
- Intermediate Dry AMD: More noticeable drusen and mild changes to central vision.
- Late Dry AMD (Geographic Atrophy): Includes the death of light-sensitive cells and significant central vision loss.
Progression to Wet AMD
Any stage of dry AMD can progress to the wet form, marked by the growth of fragile new blood vessels that bleed or leak fluid. Wet AMD always represents a late and advanced stage, and can result in rapid and severe vision loss if untreated.
Symptoms of AMD
Many people with early AMD experience no or very few symptoms. As the disease progresses, central vision may deteriorate noticeably. Common symptoms include:
- Blurry or fuzzy central vision
- Difficulty reading or seeing fine details, even with corrective lenses
- Distorted vision: Straight lines may appear wavy or bent (metamorphopsia)
- Dark or empty areas in the center of vision
- Difficulty recognizing faces
- Need for brighter light when reading or performing close tasks
Notably, peripheral vision usually remains unaffected, so people retain the ability to move around even as the central field is compromised.
Risk Factors for Age-Related Macular Degeneration
While no one can completely avoid aging, several risk factors can influence both the likelihood of developing AMD and the rate of progression. Among the most significant are:
- Age: The risk rises sharply after age 50.
- Family history: Genetics play a role; having a close relative with AMD increases risk.
- Smoking: Smoking is the single most significant modifiable risk factor and doubles the risk of AMD onset and progression.
- Race and ethnicity: Caucasians are at higher risk than other populations.
- Cardiovascular health: High blood pressure, high cholesterol, and obesity are associated with increased risk.
- Diet: Diets high in saturated fats or low in leafy green vegetables and antioxidants may elevate risk.
- Sun exposure: Excessive, unprotected exposure to ultraviolet light may increase the likelihood of developing AMD.
- Gender: Women, particularly those post-menopause, appear to have a slightly higher risk compared to men.
How Is AMD Diagnosed?
Early diagnosis of AMD is vital in managing the disease and slowing its progression. Because symptoms may not manifest in the early stages, comprehensive eye examinations are essential, particularly for individuals over 50 or with other risk factors. Diagnosis may include the following steps:
- Dilated Eye Exam: The eye care professional uses eye drops to widen (dilate) the pupil, allowing a better view of the macula and retina.
- Fundus Photography: High-resolution images of the retina are captured to document drusen, pigment changes, or other signs of AMD.
- Optical Coherence Tomography (OCT): A non-invasive scan that produces detailed cross-sectional images of the retina, revealing thinning or swelling of macular layers, and fluid or blood beneath the retina for wet AMD diagnosis.
- Fluorescein Angiography: A special dye is injected into a vein; as it travels through the retina, it highlights abnormal blood vessels or leakage typical of wet AMD.
- Amsler Grid Test: A simple, self-administered tool that helps detect central vision distortion or changes; a grid of straight lines is observed for waves, blurs, or missing spots.
Self-Monitoring: The Amsler Grid
The Amsler grid can help people with AMD notice subtle vision distortions or changes at home. By checking the grid regularly (ideally daily), individuals can detect the earliest signs of disease progression. Any sudden change warrants immediate contact with an eye care provider.
Prevention and Risk Reduction
Although AMD cannot be completely prevented, several lifestyle modifications can reduce the risk or slow the disease’s progress:
- Quit smoking: Smokers are up to four times more likely to develop AMD than non-smokers.
- Maintain a healthy diet rich in leafy greens, colorful vegetables, fruits, whole grains, lean proteins, and omega-3 fatty acids.
- Control blood pressure, cholesterol, and body weight through regular exercise and healthy eating.
- Wear UV-blocking sunglasses to limit exposure to harmful ultraviolet light.
- Schedule regular eye exams, especially if aged 50 or older or if AMD runs in the family.
Treatment Options for AMD
Treatment strategies for AMD depend on the type (dry or wet) and the disease stage. While early dry AMD has no established treatment, lifestyle modifications and certain supplements can slow its progress. Wet AMD, though more severe, has several effective medical interventions:
Treating Dry AMD
- No cure currently exists for early or intermediate dry AMD.
- AREDS/AREDS2 Supplements: Large studies recommend a specific combination of antioxidants and minerals—vitamins C and E, zinc, copper, lutein, and zeaxanthin—which slow progression in people with intermediate or late AMD in one eye.
- Visual aids and adaptive devices can help those with central vision loss maintain independence.
Treating Wet AMD
- Anti-VEGF Injections: Medications injected into the eye (such as ranibizumab, aflibercept, or bevacizumab) block vascular endothelial growth factor (VEGF), reducing abnormal blood vessel growth and fluid leakage.
- Laser Therapy: High-energy lasers can seal leaking blood vessels in select cases.
- Photodynamic Therapy (PDT): A light-sensitive drug is injected into the bloodstream and activated by a laser in the eye to close abnormal vessels.
- Surgery: Occasionally, surgery may be necessary for severe bleeding or other complications.
Prompt treatment of wet AMD is critical to preserving remaining vision. Delays can result in rapid and permanent loss of central vision.
Living with AMD: Coping Strategies and Support
While AMD can significantly affect daily living, many people maintain active, independent lives with the help of resources and support. Key coping mechanisms include:
- Low Vision Rehabilitation: Specialists can recommend training and devices to maximize remaining vision, such as magnifiers, high-contrast reading material, or text-to-speech technologies.
- Environmental Modifications: Improved lighting, high-contrast labels or markings, and simplifying indoor layouts enhance safety and usability.
- Support Groups: In-person or online communities offer emotional support, information, and practical advice for living with AMD.
- Assistive Technology: Talking clocks, audiobooks, and digital voice assistants can help compensate for vision loss.
Frequently Asked Questions (FAQs)
What is the difference between dry and wet AMD?
Dry AMD is a slower, progressive degeneration due to the thinning of the macula and accumulation of drusen. Wet AMD is more aggressive and results from abnormal blood vessel growth under the retina, leading to sudden and severe vision changes.
If I have AMD in one eye, will I get it in the other?
People with AMD in one eye have a higher risk of developing the disease in the other, though progression rates may vary. Regular monitoring is vital for both eyes.
Can AMD be prevented?
While aging and genetics cannot be changed, not smoking, managing health conditions, and consuming protective nutrients may reduce risk or slow progression.
Does AMD lead to total blindness?
AMD does not typically cause complete blindness, as peripheral vision remains. However, loss of central vision can make critical tasks like reading or recognizing faces difficult.
What should I do if I notice vision changes?
Report any sudden changes—such as blurred vision or distortion—to an eye care professional immediately. Early intervention is critical for effective treatment, especially for wet AMD.
Additional Resources and Support
- Regular consultations with an ophthalmologist or optometrist
- Low vision rehabilitation services
- Support groups for people with vision impairment
- Amsler grid (available through most eye care providers for self-monitoring)
AMD Types and Comparison Table
| Feature | Dry AMD | Wet AMD |
|---|---|---|
| Prevalence | 80–90% of cases | 10–20% of cases |
| Progression | Slow, over years | Rapid, over weeks/months |
| Cause | Thinning of macula and drusen | Abnormal, leaky blood vessels |
| Symptoms | Gradual central vision loss | Sudden, severe vision distortion or loss |
| Treatment | AREDS/AREDS2 supplements | Anti-VEGF injections, laser, PDT |
Key Takeaways
- AMD is a major cause of vision loss among adults over 50 but rarely results in total blindness.
- Early, regular eye exams are the best defense, as symptoms often go unnoticed until the disease has progressed.
- While no cure exists for AMD, many interventions can slow its course and preserve vision.
- Healthy lifestyle choices—especially not smoking—are critical for reducing risk.
- Living well with AMD is possible thanks to support services, vision rehabilitation, and adaptive technologies.
References
- https://www.californiaretina.com/blog/early-signs-and-symptoms-of-age-related-macular-degeneration-what-to-look-for
- https://www.mdfoundation.com.au/about-macular-disease/age-related-macular-degeneration/amd-overview/
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration
- https://my.clevelandclinic.org/health/diseases/15246-macular-degeneration
- https://medlineplus.gov/maculardegeneration.html
- https://www.nhs.uk/conditions/age-related-macular-degeneration-amd/symptoms/
- https://health.ucdavis.edu/blog/cultivating-health/macular-degeneration-stages-symptoms-and-when-to-get-an-eye-exam/2024/06
- https://www.mayoclinic.org/diseases-conditions/dry-macular-degeneration/symptoms-causes/syc-20350375
- https://www.youtube.com/watch?v=YoDR0A9xo8I
Read full bio of medha deb












