Understanding Acute Promyelocytic Leukemia: Symptoms, Diagnosis, and Treatment
Explore the symptoms, diagnosis, and advanced treatments for acute promyelocytic leukemia, a unique and highly treatable form of blood cancer.
Understanding Acute Promyelocytic Leukemia (APL)
Acute promyelocytic leukemia (APL) is a distinct and aggressive subtype of acute myeloid leukemia, a cancer of the blood and bone marrow involving an abnormal proliferation of immature white blood cells called promyelocytes. With specialized treatment protocols, APL has shifted from being one of the most fatal to one of the most curable forms of leukemia in recent decades. This article provides an in-depth overview of APL, focusing on its symptoms, causes, risk factors, diagnosis, treatment, and prognosis, as well as addressing frequently asked questions about the disease.
What Is Acute Promyelocytic Leukemia?
Acute promyelocytic leukemia (APL) is a rare but critical form of acute myeloid leukemia (AML) characterized by the rapid accumulation of abnormal white blood cells known as promyelocytes in the bone marrow. This accumulation interferes with the production of healthy blood cells, leading to symptoms caused by anemia, thrombocytopenia (low platelets), and leukopenia (low normal white cells). APL is most notably associated with a serious bleeding disorder (coagulopathy) due to both low platelet count and the release of clotting substances by the malignant cells, putting patients at risk of life-threatening bleeding and abnormal clotting.
- APL accounts for about 600 to 800 new cases per year in the United States.
- Most commonly diagnosed in adults around 40 years old, but can occur at any age, including children.
- The hallmark of APL is a genetic translocation involving the PML and RARα genes, resulting in the PML-RARα fusion protein.
Symptoms of Acute Promyelocytic Leukemia
APL symptoms arise primarily from the lack of healthy blood cell production and the unique coagulopathy associated with this distinct leukemia. In its early stages, APL may present much like other types of leukemia but is rapidly distinguishable by its prominent bleeding and clotting tendencies.
Common Signs and Symptoms
- Easy bruising and excessive bleeding: Nosebleeds, bleeding gums, blood in urine (hematuria), heavy menstrual periods, bleeding in the gut (black or red stool), or difficulty stopping bleeding from minor cuts.
- Petechiae: Tiny red or purple spots under the skin due to bleeding from small blood vessels.
- Fatigue and weakness: Often resulting from anemia (low red blood cell count).
- Pallor: Noticeable paleness of the skin and mucous membranes.
- Frequent infections: Due to low levels of normal, infection-fighting white blood cells.
- Fever, chills, and night sweats: Often referred to as “B symptoms” in leukemia.
- Unintentional weight loss and loss of appetite
- Bone and joint pain: Caused by accumulation of leukemic cells in these tissues.
Symptoms Related to Bleeding and Clotting Disorders
- Hemorrhage: Bleeding in the brain can cause headaches, confusion, difficulty speaking, or problems moving parts of the body — a medical emergency.
- Gastrointestinal bleeding: May present as black, tarry stool or blood streaks in stool.
- Blood clots (thrombosis): Paradoxically, patients may also develop abnormal blood clots, leading to swelling, pain, or, if clots travel to the lungs, chest pain and breathing difficulty.
Fatigue
Fatigue in APL can be profound and persistent, often unrelated to rest. It most commonly results from anemia but may also stem from overall poor health and infection.
Infections
With low numbers of mature white blood cells, patients are at increased risk for both frequent and severe infections, emphasizing the importance of monitoring for fever or signs of infection and seeking medical help promptly.
Causes and Risk Factors
APL arises from genetic changes in the DNA of immature white blood cell precursors. The defining factor of APL is a specific chromosomal rearrangement, most often a translocation between chromosomes 15 and 17. This translocation creates the PML-RARα fusion gene, which disrupts normal white blood cell development, causing promyelocytes to accumulate.
- The exact cause of this genetic change is unknown.
- Most people diagnosed have no clear risk factors or inherited predisposition.
- There is no strong evidence linking APL to environmental exposures, prior chemotherapy, or radiation therapy, in contrast to some other leukemia types.
Diagnosis of Acute Promyelocytic Leukemia
Prompt diagnosis of APL is crucial since its coagulopathy can lead to life-threatening bleeding early in the disease. Diagnosis typically involves several steps:
Medical History and Physical Examination
- Detailed assessment of symptoms such as unexplained bleeding, bruising, infections, and fatigue.
- Physical exam may reveal petechiae, pallor, or signs of active bleeding.
Laboratory Tests
- Complete Blood Count (CBC): Usually shows low platelet count, low red blood cells, and abnormal white cell counts.
- Blood chemistry and coagulation studies: Assess for clotting abnormalities.
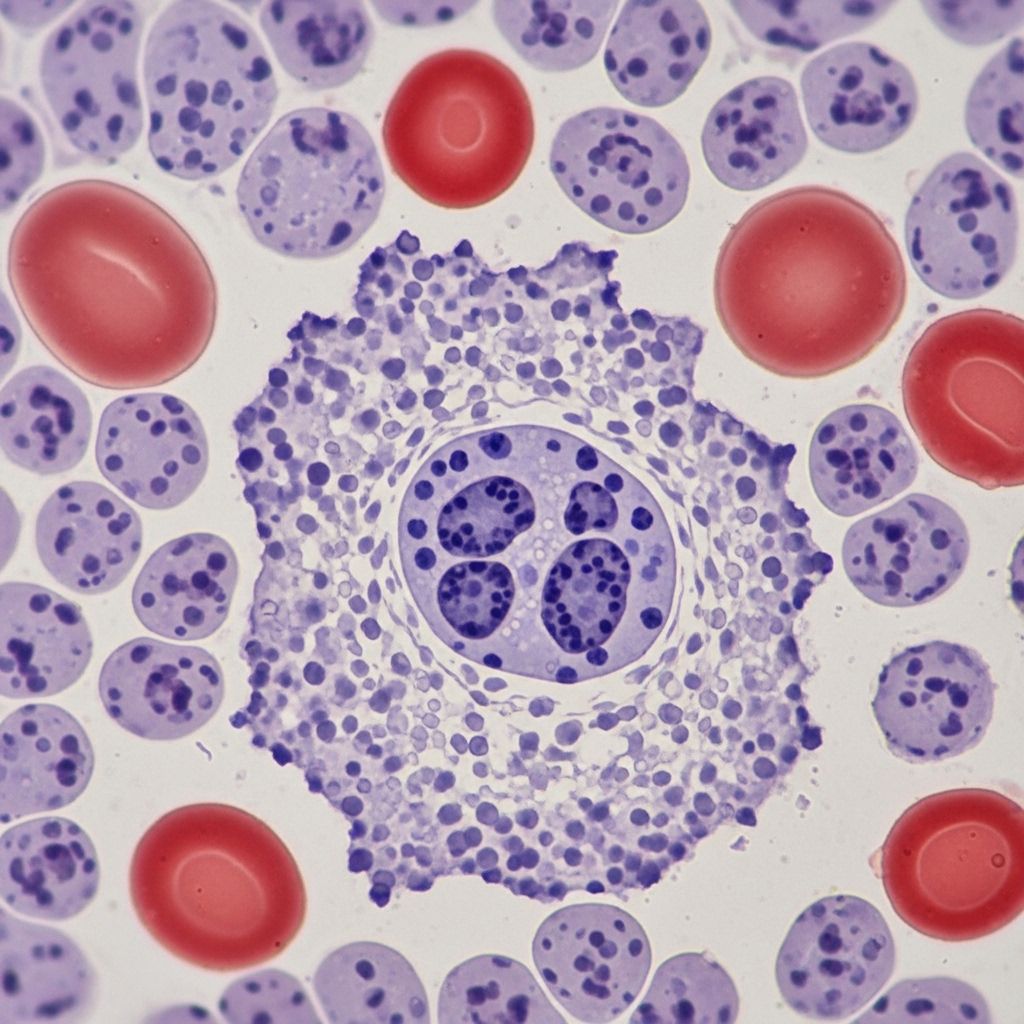
Bone Marrow Aspiration and Biopsy
- Essential to confirm diagnosis by visualizing excess promyelocytes in the bone marrow.
- Typical findings include heavy infiltration of promyelocytes and evidence of abnormal maturation.
Genetic and Molecular Tests
- Cytogenetic analysis: Identifies the characteristic t(15;17) chromosomal translocation.
- Polymerase Chain Reaction (PCR) and Fluorescence In Situ Hybridization (FISH): Detects the PML-RARα fusion gene, the molecular hallmark of APL.
| Test | Findings |
|---|---|
| Blood count | Low platelets, low red cells, abnormal white cells |
| Bone marrow exam | Promyelocyte-rich infiltration |
| Cytogenetics | t(15;17) translocation |
| Molecular studies | PML-RARα fusion gene |
Treatment Options for Acute Promyelocytic Leukemia
APL is a medical emergency due to its coagulopathy and must be started on treatment as soon as the disease is suspected, often even before genetic confirmation. Treatment strategies have evolved dramatically, and current protocols achieve remission in the vast majority of cases.
Acute Phase (Induction Therapy)
- All-trans retinoic acid (ATRA): A non-chemotherapy differentiating agent that encourages promyelocytes to mature and stop dividing. ATRA directly targets the PML-RARα fusion protein.
- Arsenic trioxide: Promotes degradation of the abnormal fusion protein and maturation of promyelocytes.
- Chemotherapy: Low-dose chemotherapy drugs may be added, especially in high-risk cases.
- Supportive care: Platelet and clotting factor transfusions to manage bleeding risk, antibiotics for infections, and careful monitoring in a hospital setting.
Consolidation Therapy
- After remission (disappearance of detectable leukemic cells), additional cycles of ATRA, arsenic trioxide, and sometimes chemotherapy are given to eliminate any remaining cancer cells and stabilize remission.
Maintenance Therapy
- Purpose: Reduce the risk of relapse, especially in patients at higher risk.
- Typical agents: Intermittent ATRA, low-dose chemotherapy, or a combination over several years.
Supportive and Emergency Management
- Transfusions: Platelets and clotting factors, red blood cells as needed.
- Intrathecal chemotherapy: Delivered into spinal fluid if there is concern for spread to the brain (uncommon in APL).
Prognosis and Outlook
A diagnosis of APL was once associated with poor survival, primarily due to the high risk of fatal bleeding at presentation. Modern treatment, however, has profoundly improved outcomes:
- With rapid initiation of ATRA and arsenic trioxide, remission rates exceed 90%.
- Many patients achieve long-term survival and potential cure.
- Risk of serious complications is highest in the first phase before and during early treatment, underscoring the need for rapid diagnosis and specialized care.
Potential Complications
- Coagulopathy: Persistent risk of hemorrhage and thrombosis until disease is controlled. Early death is most often due to bleeding in the brain or lungs, making prompt therapy vital.
- Differentiation syndrome: A potentially life-threatening reaction to ATRA or arsenic trioxide, with symptoms such as fever, fluid buildup, and lung distress requiring urgent treatment with steroids.
- Infections: Due to low white blood cell counts and intensive therapy.
Living with Acute Promyelocytic Leukemia
APL treatment requires a multidisciplinary approach, including oncology, hematology, supportive care, and rehabilitation specialists. Emotional and psychological support, infection prevention, and long-term follow-up are crucial for maintaining quality of life during and after treatment.
Tips for Coping and Support
- Attend all scheduled medical appointments and report symptoms promptly.
- Follow infection prevention measures: hand hygiene, avoiding crowds, and vaccinations as advised.
- Seek support from mental health professionals, social workers, or patient advocacy organizations.
- Maintain good nutrition and rest.
Frequently Asked Questions (FAQs)
What distinguishes APL from other types of leukemia?
APL is uniquely defined by the PML-RARα gene fusion, unique coagulopathy, and its high sensitivity to differentiating agents like ATRA and arsenic trioxide. Unlike most AML subtypes, APL requires urgent specialized intervention due to the bleeding risk.
Is APL curable?
With current protocols, the majority of patients enter complete remission, and long-term survival rates are high. Cure is possible in a significant proportion, especially when therapy is initiated rapidly.
What is the most dangerous complication of APL?
The most immediate threat is life-threatening bleeding due to coagulopathy at or soon after diagnosis. Differentiation syndrome later in therapy is also a serious but manageable risk with proper monitoring and treatment.
Can children get APL?
Yes, while most diagnoses are in adults around age 40, APL can also occur in children.
Are there known risk factors or causes?
Most cases develop without a clear cause or risk factor. There is no solid evidence linking APL to environmental exposures or lifestyle, and it is not considered an inherited condition.
Can APL relapse after remission?
Relapse is less common today with modern therapies, especially when patients complete prescribed consolidation and maintenance therapy. Continued follow-up is necessary to monitor for recurrence.
Summary Table: Acute Promyelocytic Leukemia at a Glance
| Aspect | Details |
|---|---|
| Incidence | Rare, 600–800 new annual cases in the US |
| Median Diagnosis Age | ~40 years (can occur at any age) |
| Genetic Marker | PML-RARα gene fusion (t(15;17)) |
| Main Symptoms | Bleeding, bruising, fatigue, infections, fevers |
| Main Treatment | ATRA, arsenic trioxide, chemotherapy, supportive care |
| Prognosis | Excellent with rapid diagnosis and modern treatment; long-term survival common |
Further Resources and Support
- Leukemia & Lymphoma Society: Educational materials, support programs, and guidance.
- Blood Cancer UK: Information, patient forums, and community support.
- National Organization for Rare Disorders (NORD): Advocacy and connections to rare cancer resources.
References
- https://www.moffitt.org/cancers/acute-promyelocytic-leukemia-apl/
- https://medlineplus.gov/genetics/condition/acute-promyelocytic-leukemia/
- https://bloodcancer.org.uk/understanding-blood-cancer/leukaemia/acute-promyelocytic-leukaemia/apl-symptoms/
- https://rarediseases.org/rare-diseases/acute-promyelocytic-leukemia/
- https://www.medicalnewstoday.com/articles/acute-promyelocytic-leukemia
- https://my.clevelandclinic.org/health/diseases/acute-promyelocytic-leukemia
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6303006/
- https://www.mskcc.org/cancer-care/types/leukemias/types/acute-promyelocytic-leukemia-apl
- https://bloodcancer.org.uk/understanding-blood-cancer/leukaemia/acute-promyelocytic-leukaemia/
Read full bio of Sneha Tete












