Acute Myeloid Leukemia (AML) Treatment Options: What to Expect
A comprehensive overview of treatments, expectations, and supportive care for adults with acute myeloid leukemia.
Acute Myeloid Leukemia (AML) Treatment: What to Expect
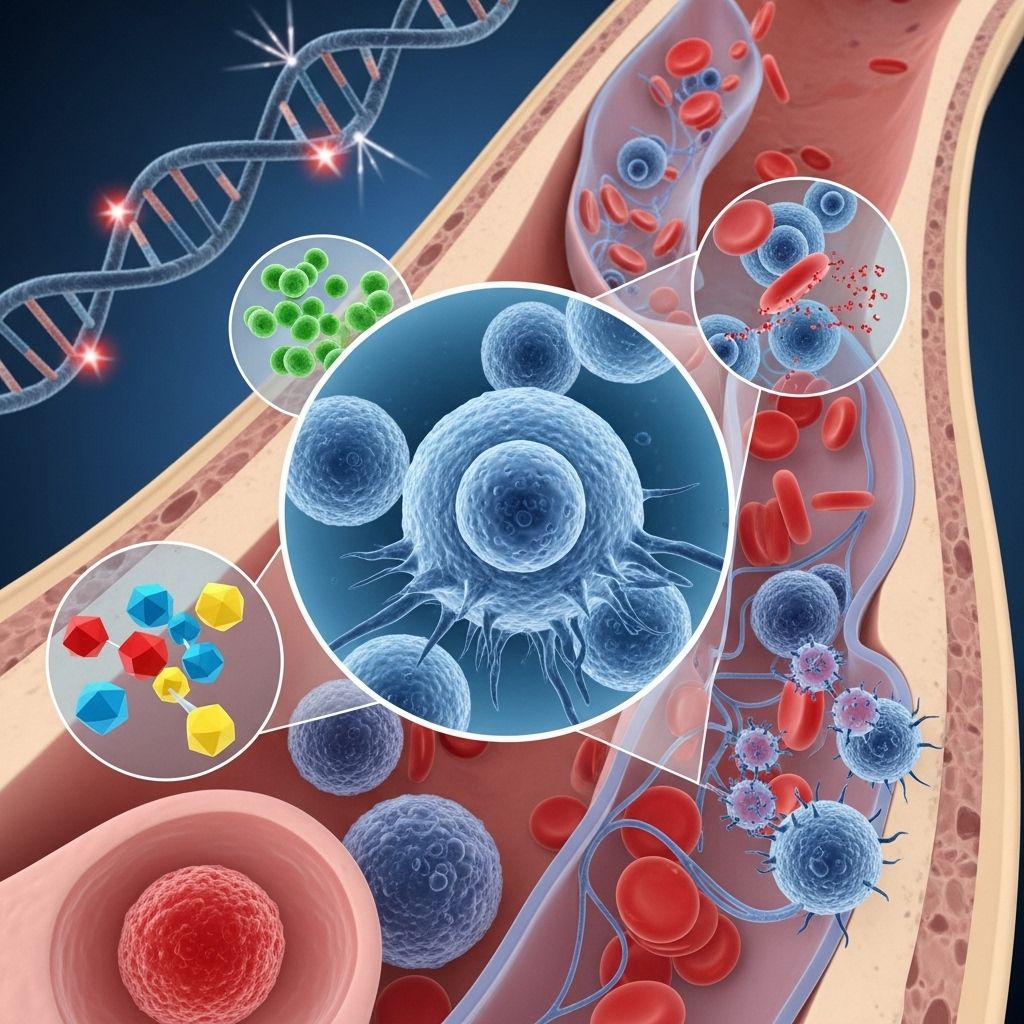
Acute myeloid leukemia (AML) is a fast-growing cancer that affects the blood and bone marrow. Its aggressive nature means treatment must often start soon after diagnosis, tailored to each patient’s AML subtype, age, health, and overall preferences. This article provides a detailed guide to the main treatment strategies, what to expect during care, and the supportive therapies often required to manage AML and its related effects.
Understanding AML Treatment Phases
Treatment for AML typically occurs in two main phases:
- Remission Induction Therapy: The initial phase, aimed at destroying as many leukemia cells as possible in the blood and bone marrow. The goal is to achieve remission, where no visible signs of leukemia remain and blood counts return to normal ranges.
- Consolidation (or Postremission) Therapy: Begins once remission is achieved. This critical phase targets any remaining leukemia cells that may not be detectable but could cause a relapse if left untreated. Consolidation therapy is sometimes called maintenance therapy, though true maintenance therapy is uncommon in AML compared with some other leukemia types.
How Treatment Is Decided
Doctors consider several factors to recommend the most appropriate AML treatment plan:
- AML subtype and genetic mutations (e.g., presence of FLT3, IDH1, or IDH2 mutations)
- Patient’s age and fitness level
- Existing health conditions and risk factors
- Prior history of treatments, if any
- Patient’s goals, wishes, and preferences
Intensive therapy is often given to people able to tolerate it, while non-intensive approaches are available for older adults or those with additional health challenges.
Core Treatment Options for AML
Chemotherapy
Chemotherapy is the backbone of AML therapy. It uses powerful drugs to kill rapidly-dividing cells, targeting leukemia throughout the body.
- Typically administered as a combination of two or more drugs. Common regimens include cytarabine plus an anthracycline (such as daunorubicin or idarubicin).
- Chemotherapy is delivered intravenously (IV) and may require a hospital stay, especially during the first phase due to significant drops in healthy blood cells and infection risk.
- Additional drugs, such as midostaurin (for patients with FLT3 mutations), may be combined with chemotherapy as a targeted approach.
- For patients who cannot tolerate intense chemotherapy, lower-dose options (such as low-dose cytarabine, azacitidine, or decitabine) may be used, sometimes alongside targeted drugs (e.g., >venetoclax< or >glasdegib<).
Common Side Effects of Chemotherapy
- Nausea and vomiting
- Hair loss
- Fatigue
- Greater risk of infections due to lowered white blood cell counts
- Increased bleeding or bruising (from low platelets)
- Potential long-term complications: heart or lung problems, fertility issues, risk of developing other cancers
Targeted Therapy
Targeted therapies attack specific molecules or genetic mutations involved in AML growth and survival. They may be used alone or in combination with chemotherapy, particularly in patients with certain genetic mutations.
- FLT3 inhibitors (e.g., midostaurin, gilteritinib, quizartinib): Used if the leukemia harbors FLT3 gene mutations.
- IDH1/IDH2 inhibitors (e.g., ivosidenib for IDH1 mutations, enasidenib for IDH2 mutations)
- Venetoclax: Used with low-dose chemotherapy in patients unsuitable for intensive therapy.
- Gemtuzumab ozogamicin: An antibody-drug conjugate that delivers chemotherapy directly to leukemia cells, used in specific cases.
Bone Marrow or Stem Cell Transplant
A stem cell (bone marrow) transplant involves replacing unhealthy bone marrow with healthy stem cells to establish new, leukemia-free blood cell production. It may be recommended for those with higher-risk disease or residual leukemia after initial therapy.
- Allogeneic transplant: Uses stem cells from a matching, healthy donor. Most common type for AML.
- Autologous transplant: Uses the patient’s own stem cells (less common in AML).
- Typically performed after high-dose chemotherapy (conditioning regimen) to eradicate any remaining leukemia cells.
- Significant risks include infections, graft-versus-host disease (GVHD), and other complications from intense immune suppression.
Radiation Therapy
Radiation uses high-energy x-rays to kill cancer cells. While not a mainstay in AML, it may be used:
- If leukemia has spread to the brain, spine, or other sanctuary sites
- As part of preparation for stem cell transplant
Leukapheresis
Leukapheresis is a procedure to rapidly lower extremely high white blood cell counts by filtering excess cells from the blood. It is used as a temporary measure, often before starting chemotherapy, to reduce the risk of complications from high white cell counts (such as blood vessel blockages).
Clinical Trials
Clinical trials offer patients access to new and emerging therapies not yet widely available, such as novel targeted agents, immunotherapies, or unique combinations of existing drugs. Participation may be especially encouraged for patients with relapsed or refractory AML, or when standard treatments are less effective.
Supportive Care During Treatment
Because AML treatments can be very aggressive and often lead to critically low blood counts, supportive care is a vital component of the overall treatment plan. Support measures are required not only to improve comfort but also to increase the likelihood of treatment success.
- Blood transfusions: Red blood cell or platelet transfusions to manage anemia and prevent bleeding complications.
- Antibiotics and antifungals: Prophylactic or therapeutic use to treat or prevent infections due to immune suppression.
- Growth factor injections: Stimulate production of new blood cells.
- Pain and symptom management: Treats side effects such as nausea, mouth sores, and fatigue.
What to Expect During AML Treatment
Treatment for AML is typically intense, with hospitalization common during the initial phase to manage side effects and monitor for complications. Testing and evaluations are frequent, including blood counts, bone marrow biopsies, and infection surveillance.
- Length and intensity of treatment: Varies based on therapy chosen and patient factors, but induction usually requires several weeks. Consolidation therapy may be spaced over several cycles, often delivered as an outpatient for patients who tolerate treatment well.
- Potential complications: Infections, bleeding, organ dysfunction, and the potential need for intensive care support during severe illness phases.
Side Effects and Late Effects of AML Treatment
AML treatments can cause both short-term and long-term side effects. Immediate issues during therapy may include :
- Low red blood cells (anemia)
- Low platelets (thrombocytopenia)
- Low white blood cells (neutropenia, increasing infection risk)
In the long term, some patients may develop:
- Heart or lung problems
- Second cancers, due to some chemotherapy drugs
- Fertility issues
- Chronic fatigue or pain
Supportive measures, regular surveillance, and lifestyle adaptations can help manage these risks.
Prognosis and Outlook
Success rates and outlook for AML depend on multiple factors:
- Genetic and molecular subtype of AML
- Patient age and overall fitness
- Response to initial therapy (achievement of remission)
- Eligibility for and results of stem cell transplantation
- Whether the leukemia returns after treatment (relapse)
Frequently Asked Questions (FAQs)
What are the main phases of AML treatment?
The two key phases are remission induction (to achieve absence of detectable leukemia) and consolidation therapy (to eliminate any remaining cancer cells and prevent relapse).
Can older adults receive the same treatments as younger patients?
Older adults or those with other health conditions may not tolerate intensive therapies. Less-intensive or palliative treatment approaches are often available and tailored to individual needs.
Are bone marrow transplants always necessary?
Not all AML patients require a bone marrow transplant. Transplants are typically reserved for those at higher risk of relapse or those with poor prognostic markers, but many can achieve durable remissions with chemotherapy and targeted therapy alone.
What is the role of supportive care in AML?
Supportive care is essential to manage treatment side effects, such as infection, bleeding, and anemia; it helps keep patients well enough to continue therapy and reduces treatment complications.
Are there new treatments or clinical trials for AML?
Yes. Clinical trials are testing new targeted therapies, immunotherapies, and novel drug combinations for AML, offering hope for better outcomes, especially in patients with hard-to-treat cases or relapsed disease.
Summary Table: Main AML Treatment Options
| Treatment | Description | When Used | Risks/Side Effects |
|---|---|---|---|
| Chemotherapy | Drugs that kill leukemia cells | First-line for most AML | Nausea, infections, hair loss, bleeding |
| Targeted Therapy | Drugs targeting specific mutations | Subtypes with FLT3, IDH1/2, others | Similar to chemo, with unique risks |
| Stem Cell Transplant | Healthy donor or self stem cells replace marrow | High-risk or relapsed AML post-chemo | Infections, GVHD, significant side effects |
| Radiation Therapy | Targeted x-rays destroy leukemia in sanctuary sites | Spread to brain/CNS or transplant preparation | Skin burns, fatigue, localized side effects |
| Leukapheresis | Mechanical removal of excess white blood cells | Very high white counts pre-chemo | Bleeding, infection risk |
Key Takeaways
- AML is an aggressive leukemia type that requires prompt, individualized treatment plans.
- Treatment phases include induction to achieve remission and consolidation to prevent relapse.
- Core treatments: chemotherapy, targeted drugs, stem cell transplantation, radiation (for certain situations), and supportive care.
- Managing side effects and maintaining quality of life are vital components of a patient’s overall therapy.
- Clinical trials are important for accessing new options and advancing AML care.
References
- https://www.mayoclinic.org/diseases-conditions/acute-myelogenous-leukemia/diagnosis-treatment/drc-20369115
- https://www.mskcc.org/cancer-care/types/leukemias/treatment/acute-myeloid-leukemia
- https://www.cancer.gov/types/leukemia/patient/adult-aml-treatment-pdq
- https://www.cancerresearchuk.org/about-cancer/acute-myeloid-leukaemia-aml/treating-aml
- https://vicc.org/cancer-info/adult-acute-myeloid-leukemia
- https://www.cancer.org/cancer/types/acute-myeloid-leukemia/treating.html
- https://my.clevelandclinic.org/health/diseases/6212-acute-myeloid-leukemia-aml
- https://www.nhs.uk/conditions/acute-myeloid-leukaemia/treatment/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10256410/
Read full bio of medha deb












