Acute Myelogenous Leukemia: Causes, Symptoms, Diagnosis, and Treatment
Your comprehensive guide to understanding acute myelogenous leukemia—covering risk factors, symptoms, diagnosis, treatment, complications, and outlook.
Acute Myelogenous Leukemia (AML): Causes, Symptoms, Diagnosis, and Treatment
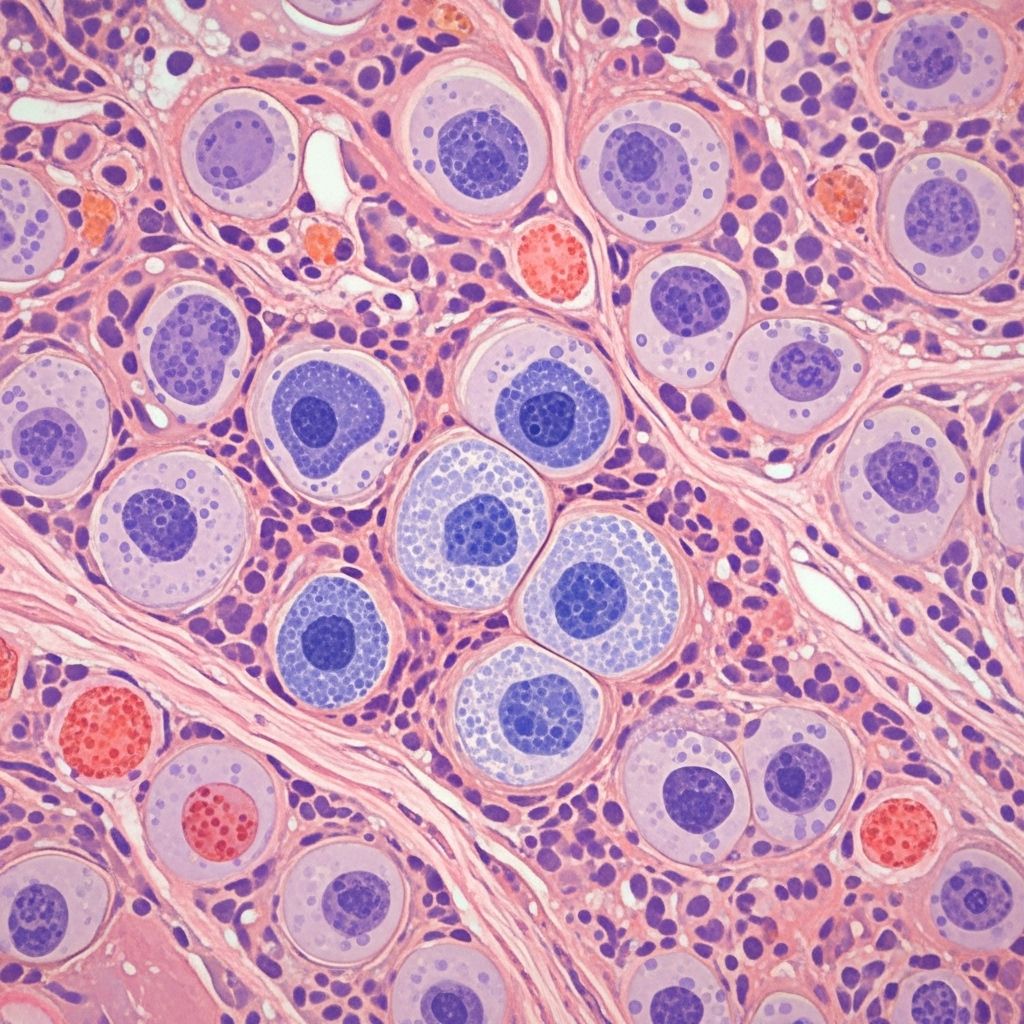
Acute myelogenous leukemia (AML) is a rapidly progressing cancer of the blood and bone marrow. The disease originates from the abnormal proliferation of immature myeloid cells, called blast cells, disrupting the normal production of healthy blood cells and leading to serious health complications if untreated.
What is Acute Myelogenous Leukemia?
AML occurs when myeloid stem cells in the bone marrow undergo genetic changes, causing them to multiply uncontrollably. This results in an accumulation of nonfunctional blasts, crowding out normal red blood cells, white blood cells, and platelets. Without effective blood cell production, the body cannot fight infection, carry oxygen efficiently, or control bleeding.
- Also known as: Acute myeloid leukemia, acute myeloblastic leukemia, granulocytic leukemia, acute nonlymphocytic leukemia
- Related conditions: Acute lymphoblastic leukemia (ALL), myelodysplastic syndromes
Who is Affected? Incidence and Age
AML can occur at any age, but most commonly affects adults over 65. The median age at diagnosis is approximately 68 years. It is rare in children and young adults, though pediatric cases do occur.
| Age Group | Approximate Frequency |
|---|---|
| Children | Uncommon |
| Adults (under 45) | Less common |
| Older Adults (65+) | Most common |
Causes of AML
AML generally arises due to genetic mutations within bone marrow stem cells, but a precise direct cause is usually not identifiable. Several risk factors increase likelihood, including:
- Previous chemotherapy or radiation therapy
- Exposure to chemicals like benzene
- Tobacco smoke
- Genetic disorders (e.g., Down syndrome, Fanconi anemia, Shwachman-Diamond syndrome)
Most cases, however, occur spontaneously without clear external causes.
Risk Factors for Developing AML
- Personal history of blood disorders (e.g., myelodysplastic syndromes)
- Family history of leukemia or genetic predispositions
- Occupational exposure to harmful chemicals or radiation
- Past cancer treatments
- Older age (risk increases with age)
Types and Classification of AML
AML is categorized by specific genetic, molecular, and morphological features of blast cells. Some types are more aggressive or respond differently to treatment. Classification helps guide therapeutic decisions and prognosis.
Symptoms of AML
Symptoms often develop rapidly over days to weeks as blast cells crowd out normal blood cells. Common signs and symptoms include:
- Fatigue and weakness
- Fever
- Paleness or pallor
- Easy bruising or bleeding (nose, gums, excessive periods)
- Frequent or persistent infections
- Shortness of breath
- Pain in bones, back, or abdomen
- Enlarged spleen or liver (sometimes causing fullness or pain below the ribs)
Symptoms overlap with common infections and other illnesses, which may complicate early diagnosis.
When to Seek Medical Help
If you experience ongoing fever, fatigue, frequent infections, easy bleeding or bruising, or other unexplained symptoms described above, consult with a healthcare provider promptly.
How is AML Diagnosed?
- Physical examination: Assessment for pallor, bruising, organ enlargement
- Blood tests: Complete blood count reveals low red cells, white cells, platelets; presence of blasts
- Bone marrow biopsy: Gold standard to confirm AML diagnosis; evaluates blast percentage and cell type
- Cytogenetic testing: Identifies chromosome mutations or abnormal genes guiding prognosis and therapy
- Flow cytometry: Distinguishes AML from related blood cancers
Is AML Staged?
Unlike most cancers, AML is not staged numerically. Instead, treatment and prognosis are based on:
- AML subtype
- Spread outside blood and bone marrow
- Previous blood disorders
- Response to prior cancer treatments
- Age and comorbidities
There is no standard staging system; the focus is on risk stratification and remission status.
Treatment Options for AML
Prompt, aggressive treatment is required due to AML’s rapid progression. Main approaches include:
- Chemotherapy: First-line and most essential treatment; aims to eliminate leukemic blast cells
- Targeted therapy: Drugs tailored to specific genetic mutations (e.g., FLT3 inhibitors)
- Stem cell (bone marrow) transplantation: Offers potential cure, especially in younger or fit patients after remission
- Supportive care: Blood transfusions, antibiotics, management of side effects
- Radiation therapy: Rarely used; may treat leukemic spread to organs
Phases of AML Treatment
- Induction therapy: Initial intensive chemotherapy designed to rapidly reduce leukemia burden
- Consolidation therapy: Additional chemo or stem cell transplant to eradicate residual disease after remission
- Maintenance therapy: Used in select cases to prevent relapse
Treatment requires skilled hospital-based care due to risks of infection, bleeding, and severe side effects.
Prognosis and Outlook for AML
Prognosis varies widely based on age, genetic mutations, response to therapy, and overall health. Key factors influencing outlook:
- Age: Younger patients generally have better survival rates
- Presence of favorable genetic markers: Certain chromosomal abnormalities predict better response
- Subtype of AML: Some types more resistant to treatment
- Coexisting health conditions: Impact tolerance of intensive therapy
Overall, approximately 30% of adults survive three or more years after diagnosis with aggressive treatment. Pediatric patients may have a five-year survival rate of 60-70% or better. Relapse is possible, especially in higher-risk subgroups.
Complications Associated with AML
- Severe infections due to low white cell counts
- Uncontrolled bleeding resulting from thrombocytopenia (low platelets)
- Anemia symptoms (fatigue, shortness of breath)
- Organ enlargement (liver, spleen), rarely infiltration of central nervous system
- Therapy-related side effects (immune suppression, organ toxicities)
Living With AML: Support and Monitoring
Managing AML requires coping with intense treatments, frequent healthcare visits, and psychological stress. Support is crucial from medical teams, social workers, and peer groups. Survivorship monitoring includes regular blood and bone marrow tests to detect potential relapse early.
Frequently Asked Questions (FAQs)
Q: What is the difference between AML and ALL?
A: AML affects myeloid cells, whereas ALL (acute lymphoblastic leukemia) affects lymphoid cells. Both are forms of acute leukemia but require different treatments and have distinct age distributions.
Q: Can AML be cured?
A: AML is potentially curable, particularly in younger patients and those who undergo successful stem cell transplant. Complete remission is achievable, but risk of recurrence exists.
Q: What is the main cause of AML?
A: Most AML cases stem from spontaneous genetic mutations. However, prior chemo/radiation, exposure to chemicals, smoking, and some inherited conditions increase risk.
Q: What are the earliest symptoms of AML?
A: The earliest signs include fatigue, frequent infections, easy bruising or bleeding, and paleness. Some may notice bone pain or abdominal discomfort from organ enlargement.
Q: How is AML different from chronic leukemia?
A: AML progresses rapidly and requires urgent intervention. Chronic leukemias develop more slowly and may be detected incidentally or monitored before therapy is started.
Q: What happens after AML treatment?
A: Patients require ongoing monitoring for relapse and management of side effects. Long-term follow-up involves blood tests, bone marrow examinations, and supportive care assessments.
Summary Table: Key Facts About AML
| Feature | Description |
|---|---|
| Disease Type | Acute blood and bone marrow cancer |
| Cell Origin | Myeloid (stem cell) lineage |
| Main Symptoms | Fatigue, infections, bleeding, bruising, anemia, pain |
| Main Treatments | Chemotherapy, stem cell transplant, targeted therapy |
| Prognosis Factors | Age, genetic markers, health, AML subtype |
| Cure Possible? | Yes, in select cases |
Supporting Resources
- National Cancer Institute: Comprehensive information on AML
- Leukemia & Lymphoma Society: Patient resources and support groups
- Mayo Clinic: Expert insights and treatment options
Final Notes
AML is a medical emergency requiring expert diagnosis and prompt, specialized treatment. Individuals affected by AML benefit from multidisciplinary care, ongoing support, and frequent monitoring for best outcomes. Advancements in targeted therapy and stem cell transplantation are improving survival rates, especially for younger or biologically favorable cases.
References
- https://www.ebsco.com/research-starters/health-and-medicine/acute-myelocytic-leukemia-aml
- https://www.medicalnewstoday.com/articles/215538
- https://www.mayoclinic.org/diseases-conditions/acute-myelogenous-leukemia/symptoms-causes/syc-20369109
- https://www.ncbi.nlm.nih.gov/books/NBK507875/
- https://www.cancer.gov/types/leukemia/patient/adult-aml-treatment-pdq
- https://www.healthline.com/health/acute-myeloid-leukemia
- https://www.healthline.com/health/leukemia/acute-myeloid-leukemia-treatment
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6105504/
- https://www.healthline.com/health/video/break-it-down-anemia-in-mds-bt
- https://my.clevelandclinic.org/health/diseases/6212-acute-myeloid-leukemia-aml
Read full bio of Sneha Tete












