Acute Lymphoblastic Leukemia (ALL) Treatment Options and Management
Explore comprehensive treatment strategies, therapies, and supportive care for acute lymphoblastic leukemia (ALL) in adults.
Acute Lymphoblastic Leukemia (ALL) Treatment: What Are Your Options?
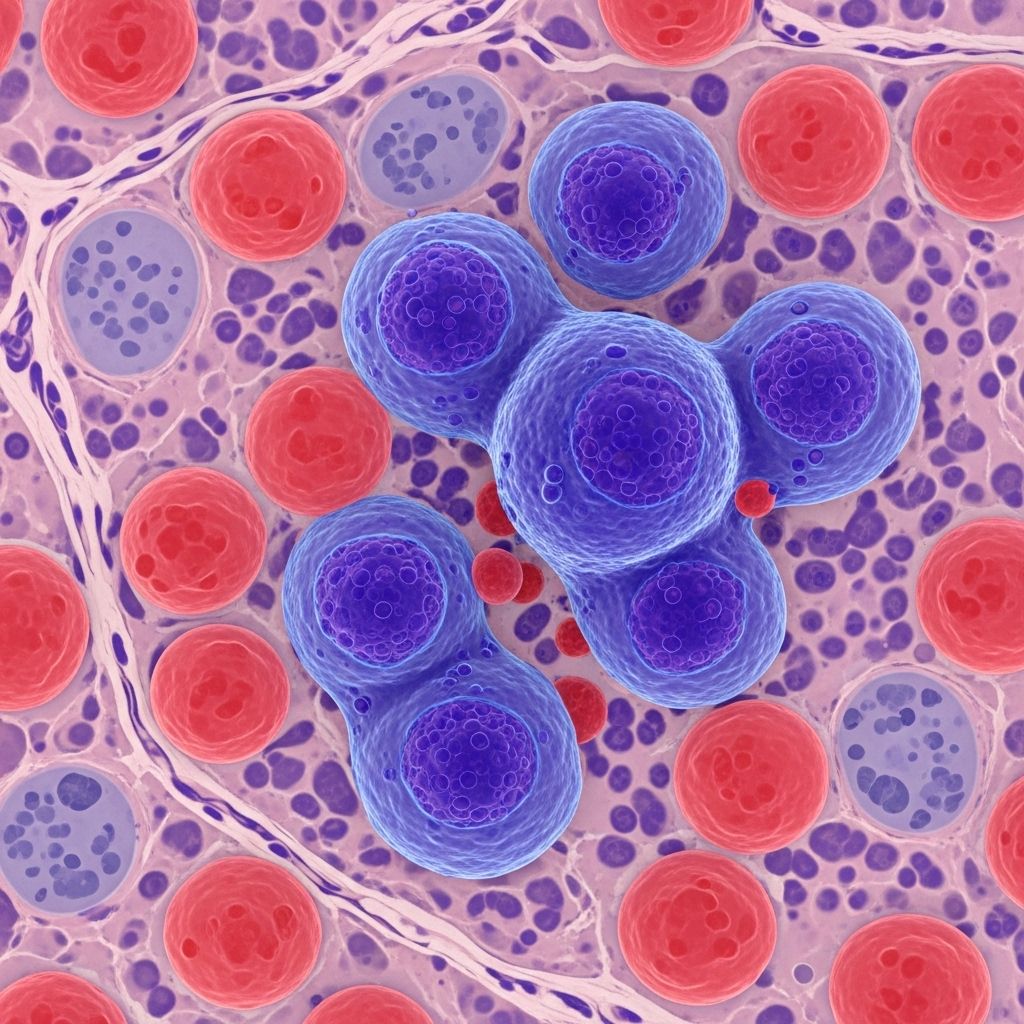
Acute lymphoblastic leukemia (ALL) is a form of cancer affecting the blood and bone marrow. Treatment strategies for ALL in adults are evolving, encompassing a variety of therapies tailored to disease type, genetic markers, risk factors, and patient health. This detailed guide explores ALL treatment phases, available therapies, and supportive care measures for those facing a diagnosis.
Quick Overview of ALL Treatment Modalities
- Chemotherapy: Mainstay of ALL treatment, usually administered in multiple phases and combinations.
- Targeted Therapy: Specially designed drugs that attack cancer cells with specific genetic mutations.
- Immunotherapy: Utilizes the body’s immune system to fight leukemia cells.
- Stem Cell Transplant: Replaces diseased bone marrow with healthy donor cells.
- Radiation Therapy: Occasionally used in select cases, such as CNS involvement or relapse.
- Clinical Trials: Access to experimental therapies.
Understanding Acute Lymphoblastic Leukemia (ALL)
ALL is an aggressive malignancy arising from immature lymphoid cells, most commonly affecting B cells or T cells. Symptoms can include fatigue, fever, weight loss, bleeding, bruising, and enlarged lymph nodes. Early and accurate diagnosis is crucial for initiating treatment.
Treatment decisions rely on:
- Cell lineage (B-cell vs. T-cell ALL)
- Genetic abnormalities, such as the Philadelphia chromosome (Ph+)
- Patient age and health
- Risk classification (standard vs. high risk of relapse)
Phases of ALL Treatment
ALL therapy traditionally follows structured phases intended to first induce remission, then eliminate residual cancer cells, and finally prevent recurrence.
| Phase | Primary Goal | Main Treatments |
|---|---|---|
| Induction | Achieve remission by killing active leukemia cells | Combination chemotherapy (may include targeted therapy) |
| Consolidation (Intensification) | Destroy remaining leukemia cells and prevent relapse | Additional chemotherapy, targeted therapy |
| Maintenance | Prevent leukemia regrowth | Low-dose chemotherapy over 1-2 years |
| CNS Prophylaxis | Prevent cancer spread to brain & spinal cord | Intrathecal or high-dose systemic chemotherapy, possible radiation |
| Stem Cell Transplant | Replace diseased marrow | Donor stem cell infusion after high-dose chemo/radiation |
| Immunotherapy | Harness immune system to destroy leukemia cells | Monoclonal antibodies, CAR-T cell therapy |
| Targeted Therapy | Inhibit growth based on specific genetic mutations | Tyrosine kinase inhibitors (TKIs) |
Chemotherapy: The Foundation of ALL Treatment
Chemotherapy remains the most frequently used and effective strategy for treating ALL, typically structured around three key phases:
- Induction: High-dose, multi-agent chemotherapy to rapidly reduce leukemia cell count.
- Consolidation (Intensification): Additional drugs or higher-dose regimens to destroy residual cancer cells.
- Maintenance: Lower-dose, prolonged chemotherapy designed to prevent relapse, with treatment duration often spanning up to two years.
Drugs used in these phases include vincristine, prednisone, asparaginase, daunorubicin, and methotrexate, among others. Regimens may be tailored based on individual risk factors, presence of CNS involvement, or disease genetics.
CNS Prophylaxis: Preventing Central Nervous System Recurrence
Leukemia cells are adept at escaping standard chemotherapy by infiltrating the central nervous system (CNS). To reduce this risk, patients receive specific interventions:
- Intrathecal chemotherapy (directly into spinal fluid)
- High-dose systemic chemotherapy
- Radiation therapy to the brain in selected cases
CNS prophylaxis is incorporated throughout all treatment phases and has substantially lowered relapse rates in the brain and spinal cord.
Targeted Therapy: Precision Medicine for Genetic Subtypes
Targeted therapies are emerging as a vital component for certain genetic subtypes. For patients whose leukemia cells express the Philadelphia chromosome (BCR-ABL mutation), tyrosine kinase inhibitors (TKIs) such as imatinib, dasatinib, or nilotinib are used alongside chemotherapy.
TKIs work by blocking the enzyme driving abnormal cell growth, helping restore healthy blood cell production. These drugs have dramatically improved outcomes in Philadelphia chromosome-positive ALL.
Immunotherapy: Harnessing the Immune System
Immunotherapy is a rapidly expanding treatment avenue for ALL, especially in refractory or relapsed cases. Available modalities include:
- Monoclonal Antibodies: Drugs such as blinatumomab (a bispecific T-cell engager) and inotuzumab ozogamicin target leukemia cells to unleash immune attack.
- CAR-T Cell Therapy: Chimeric antigen receptor (CAR) T-cell therapies, such as tisagenlecleucel and brexucabtagene autoleucel, involve genetically modifying patient T-cells to recognize and kill leukemia cells.
These therapies are offering new hope for patients with difficult-to-treat or relapsed ALL.
Stem Cell Transplant: Replacing Diseased Marrow
For individuals who do not achieve long-term remission with standard therapies—or are at high risk of recurrence—a stem cell transplant (also called bone marrow transplant) may be recommended. This procedure involves:
- High-dose chemotherapy and/or radiation to eradicate cancerous cells in the bone marrow
- Transplantation of healthy donor stem cells to restore normal blood cell production
Stem cell transplant is a high-risk but potentially curative option, often reserved for those with aggressive disease or relapse after conventional therapy.
Radiation Therapy: A Supportive Tool
Radiation therapy is generally not part of standard ALL treatment but can be used in special circumstances, such as:
- CNS involvement unresponsive to chemotherapy
- Palliative care, to mitigate symptoms in advanced disease
- Preparation for stem cell transplant
Supportive Care During ALL Treatment
Managing side effects and complications is crucial during ALL therapy. Supportive measures may include:
- Antibiotics for infection prevention
- Blood transfusions (red cells, platelets) for anemia or bleeding
- Nutritional support
- Pain management
- Palliative care for advanced disease
- Psychological and emotional support
Participating in Clinical Trials
Clinical trial participation may be offered, especially if standard therapies are unsuccessful or emergent therapies are appropriate for the patient’s disease type.
New drugs, treatment combinations, and immunotherapies are continually being studied to improve outcomes and limit toxicity.
Follow-Up Care After Treatment
Comprehensive follow-up is essential to monitor for disease recurrence, long-term side effects, and overall patient well-being. Follow-up care typically includes:
- Regular physical examinations
- Frequent blood tests and bone marrow assessment
- Management of late effects (cardiac, fertility, cognitive changes)
- Continued CNS prophylaxis, as indicated
- Psychological counseling
Most relapses occur within the first two years after treatment completion, necessitating vigilant surveillance during this time.
Frequently Asked Questions (FAQs) About ALL Treatment
How long does ALL treatment usually last?
Treatment for adult ALL typically spans 2-3 years, with the most intensive therapies administered in the first several months and maintenance therapy following for 1-2 years.
Is chemotherapy always required for ALL?
Chemotherapy is the primary cornerstone of ALL therapy; however, some patients may also receive targeted therapy, immunotherapy, or participate in stem cell transplant procedures depending on individual circumstances.
What are the major side effects of ALL treatment?
Side effects vary but can include fatigue, infections, bleeding, nausea, hair loss, and increased risk for other health issues. Supportive care and side effect management are key aspects of ALL care.
Can ALL be cured?
With advancements in chemotherapy, targeted therapy, and stem cell transplantation, a cure is possible for a significant percentage of patients—especially those who achieve and maintain remission.
How is ALL in adults different from ALL in children?
While treatment principles are similar, children generally respond better to ALL therapy and have higher cure rates. Adult ALL treatments are more likely to be tailored to genetic risk and overall health status.
Summary Table: Key Treatments for Acute Lymphoblastic Leukemia
| Treatment Type | Purpose | Common Agents/Modalities | Best for |
|---|---|---|---|
| Chemotherapy | Eliminate leukemia cells | Vincristine, cyclophosphamide, prednisone, methotrexate | All patients |
| Targeted Therapy | Block growth signals in genetically defined leukemia | TKIs: Imatinib, dasatinib, nilotinib | Ph+ (Philadelphia chromosome-positive) patients |
| Immunotherapy | Activate immune system against leukemia | Blinatumomab, inotuzumab ozogamicin, CAR-T cells | Relapsed/refractory disease |
| Stem Cell Transplant | Replace bone marrow after intensive therapy | Matched donor stem cells | High-risk or relapsed patients |
| Radiation Therapy | Treat CNS or resistant disease, palliation | External beam radiation | CNS involvement, symptom relief |
| Supportive Care | Manage side effects and complications | Transfusions, antibiotics, dietary support | All patients |
Outlook and Progress in ALL Treatment
Major strides have been made in the treatment of ALL in adults, with long-term remission now achievable for many patients due to improved chemotherapy, targeted drug options, innovative immunotherapies, and rigorous supportive care. Personalized medicine, clinical research, and ongoing monitoring continue to push the boundaries of survival and quality of life for those affected by this aggressive blood cancer.
Additional Resources
- Consult your hematologist-oncologist for individualized treatment planning.
- Explore clinical trials for access to emerging therapies.
- Leukemia & Lymphoma Society for patient support and education.
- Cancer centers’ support groups for peer connection and coping strategies.
References
- https://my.clevelandclinic.org/health/diseases/21564-acute-lymphocytic-leukemia
- https://www.mayoclinic.org/diseases-conditions/acute-lymphocytic-leukemia/diagnosis-treatment/drc-20369083
- https://www.cancer.org/cancer/types/acute-lymphocytic-leukemia/treating/typical-treatment.html
- https://www.cancer.gov/types/leukemia/patient/adult-all-treatment-pdq
- https://www.cancerresearchuk.org/about-cancer/acute-lymphoblastic-leukaemia-all/treatment
- https://www.ncbi.nlm.nih.gov/books/NBK65727/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5520400/
- https://www.stjude.org/care-treatment/treatment/childhood-cancer/leukemia-lymphoma/acute-lymphoblastic-leukemia-all.html
- https://ashpublications.org/blood/article/145/1/1/534797/Introduction-to-a-How-I-Treat-series-on-acute
Read full bio of Sneha Tete












