Acute Lymphoblastic Leukemia in Children: Causes, Symptoms, and Treatment
Understand acute lymphoblastic leukemia in children — its signs, risk factors, treatment journey, and possible outcomes.
Acute Lymphoblastic Leukemia in Children
Acute lymphoblastic leukemia (ALL) is the most common type of cancer found in children, accounting for about 30% of all pediatric cancers. This blood cancer develops rapidly, requiring prompt diagnosis and treatment. Recent advances have significantly improved survival chances for affected children, making awareness and early intervention vital.
What Is Acute Lymphoblastic Leukemia?
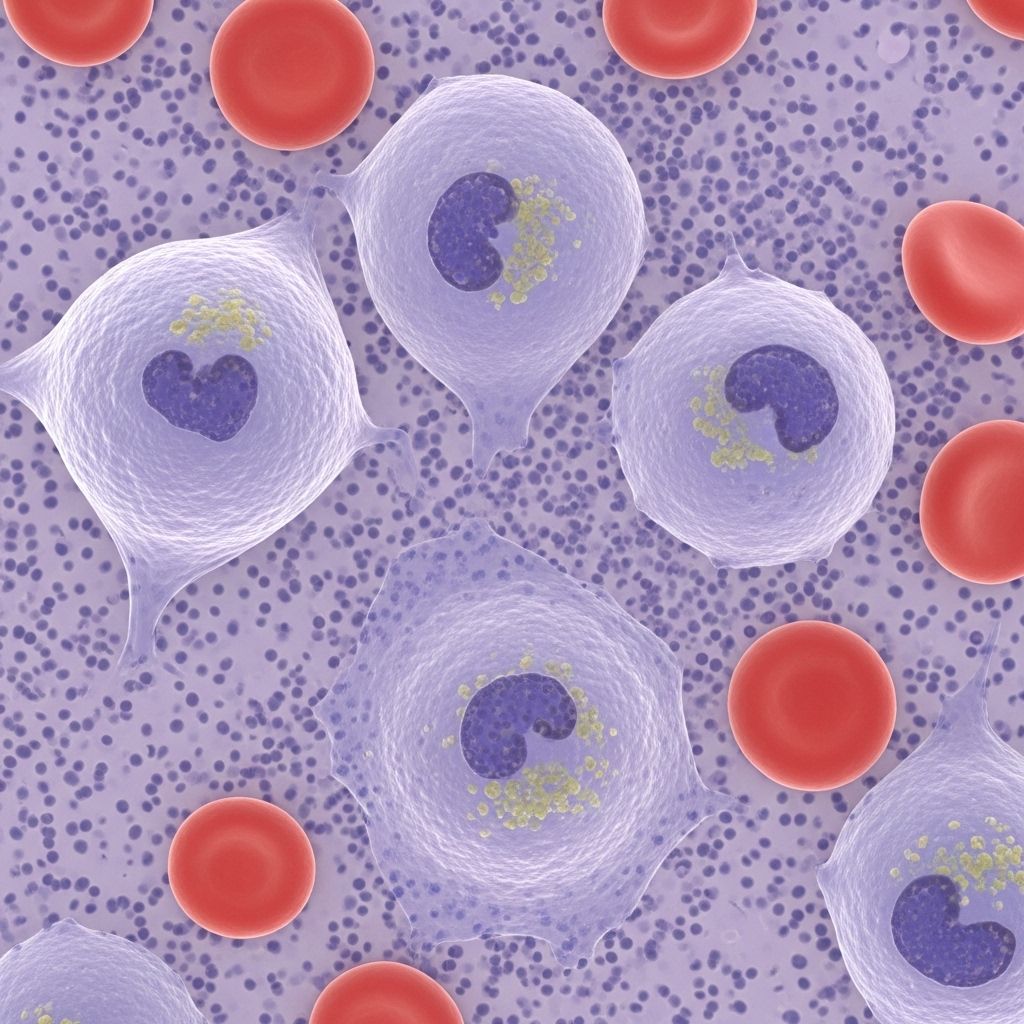
Acute lymphoblastic leukemia (ALL)—also called acute lymphocytic or acute lymphoid leukemia—is a cancer of the blood and bone marrow. The disease originates in the bone marrow, the soft tissue inside bones where blood cells are made. In ALL, the bone marrow creates too many immature white blood cells, known as lymphoblasts. These abnormal cells fail to function correctly, crowding out healthy blood cells and preventing the body from effectively fighting infections.
- ALL is acute because it develops and progresses rapidly.
- It is called lymphoblastic/lymphocytic because it impacts white blood cells called lymphocytes.
- The two primary subtypes are B-cell ALL and T-cell ALL, depending on which lymphocyte lineage is affected.
ALL is most common in children but can occur at any age. Early detection improves outcomes significantly.
How Common Is Childhood Acute Lymphoblastic Leukemia?
ALL accounts for the majority of childhood leukemia diagnoses. In the United States, approximately 3,000 cases occur annually in children and young people up to age 21. It is most frequently diagnosed between the ages of 2 and 5 years, although it can affect older children and teenagers.
- ALL represents roughly 30% of all childhood cancers.
- The disease has a high cure rate, particularly in young children when diagnosed early.
Causes and Risk Factors
The exact cause of ALL is not fully understood. Most cases do not have an identifiable risk factor or direct cause. However, several elements can increase the risk of developing ALL in children:
- Genetic conditions: Children with certain genetic syndromes—such as Down syndrome, Li-Fraumeni syndrome, neurofibromatosis, Fanconi anemia, and ataxia telangiectasia—face a higher risk.
- Family history: Having a sibling with leukemia can raise the risk slightly.
- Previous cancer treatment: Prior exposure to chemotherapy or radiation for other cancers may increase risk.
- Immune suppression: Children taking immunosuppressive drugs, for example after an organ transplant, may be more vulnerable.
- Other blood disorders: Conditions like myelodysplasia (pre-leukemia) can predispose children to ALL.
Despite these known risk factors, most children diagnosed with ALL have no clear underlying cause.
Signs and Symptoms
ALL’s symptoms develop quickly and often mimic those of common childhood illnesses. The most frequent signs include:
- Anemia: Low red blood cell count causes pallor, fatigue, weakness, and rapid heartbeat.
- Easy bruising or bleeding: Due to low platelet counts, children may bruise easily or have prolonged bleeding from minor cuts, as well as frequent or severe nosebleeds and bleeding gums.
- Bone and joint pain: Crowding in the bone marrow may cause pain, often mistaken for growing pains.
- Recurrent fevers and infections: Despite elevated white cell counts, the cells are immature, so children become more susceptible to viral and bacterial infections and may have trouble recovering from minor illnesses.
- Swollen lymph nodes: Lymph nodes in the neck, underarms, groin, or abdomen may be enlarged.
- Abdominal pain: Enlargement of organs such as the liver, spleen, or kidneys can cause abdominal pain, loss of appetite, and unexplained weight loss.
- Shortness of breath: Clusters of leukemic cells in the chest (sometimes in the thymus) can cause coughing, wheezing, or breathing difficulties—especially seen in T-cell ALL.
Other, less common, symptoms include headaches, vision problems, and difficulty with balance if leukemia cells spread to the brain or central nervous system.
When to See a Doctor
ALL symptoms can be mistaken for viral illnesses like the flu. However, if your child has persistent symptoms—especially unusual bruising, prolonged fevers, unexplained pain, or swelling—it is crucial to consult a pediatrician. Early investigation and blood tests can help rule out or diagnose ALL promptly.
How Is Acute Lymphoblastic Leukemia Diagnosed?
A prompt and accurate diagnosis is essential to start effective treatment. The diagnostic process generally includes:
- Medical history and physical examination: Checking for symptom patterns, visible signs of anemia, bruising, lymph node, or organ enlargement.
- Blood tests:
- Complete blood count (CBC) to measure levels of white and red blood cells and platelets.
- Blood smear to check for immature leukemic cells (blasts).
- Bone marrow aspiration and biopsy: Collecting bone marrow (usually from the hip bone) to confirm the presence of leukemic cells and determine their type.
- Immunophenotyping and cytogenetic analysis: Laboratory tests to classify the leukemia subtype and look for genetic changes that may guide treatment decisions.
- Lumbar puncture: Testing cerebrospinal fluid to determine if leukemia has spread to the brain or spinal cord.
- Imaging studies (if needed): Ultrasound, X-rays, CT, or MRI may be used to assess organ and lymph node involvement.
Treatment of Acute Lymphoblastic Leukemia in Children
The goal of treatment is to destroy all leukemic cells and restore normal blood cell production. The majority of children with ALL achieve remission, and many are cured. Treatment is aggressive and typically occurs in several phases:
1. Induction Therapy
The initial phase of treatment, aiming to achieve remission by killing as many leukemia cells as possible. Medications (chemotherapy) are administered intravenously, orally, and sometimes directly into the spinal fluid.
2. Consolidation (Intensification) Therapy
This phase aims to eliminate any remaining leukemia cells that could cause a relapse. It involves more intensive chemotherapy and sometimes targeted therapy based on the leukemia’s genetic features.
3. Maintenance Therapy
Low-dose chemotherapy is given over a prolonged period (often two to three years) to prevent relapse. Most of this therapy is administered orally at home, with regular clinic visits for monitoring.
Other Treatment Components
- CNS prophylaxis: Intrathecal chemotherapy is administered to prevent or treat leukemia in the brain and spinal cord, even if no evidence of spread exists at diagnosis.
- Targeted therapies: Drugs specifically designed to target genetic mutations or proteins in leukemic cells may be used in certain subtypes.
- Stem cell transplant: In high-risk cases, or if leukemia returns after initial therapy, a bone marrow or stem cell transplant may be considered.
- Supportive care: Children may need transfusions for anemia or low platelets, as well as antibiotics to combat infections.
Side Effects of Treatment
Chemotherapy and other treatments can cause both short-term and long-term side effects. The specific effects depend on the drugs used and the child’s individual tolerance. Common side effects include:
- Fatigue
- Nausea and vomiting
- Hair loss
- Mouth sores
- Increased risk of infections
- Lowered appetite and weight loss
- Bleeding or bruising easily
Most side effects resolve after treatment, but some children experience lasting effects, including learning or memory difficulties, heart or fertility issues, and higher future risk of other cancers. Ongoing follow-up is essential to monitor and address any long-term complications.
Prognosis and Survival Rates
Childhood ALL is considered highly curable. Thanks to advances in treatment protocols, the overall five-year survival rate for children diagnosed with ALL exceeds 85% in developed countries. Several factors influence prognosis:
- Age at diagnosis: Children aged 1–9 generally respond better to treatment than infants or teenagers.
- White blood cell count: Lower counts at diagnosis are typically associated with better outcomes.
- Biological markers: The presence or absence of specific genetic abnormalities affects the response to treatment.
- Early response: How quickly leukemia goes into remission after starting treatment helps predict long-term outcomes.
- Relapse risk: Children who relapse after initial treatment require more intensive or novel therapies.
Life After Treatment
Completion of therapy is a major milestone for children and families coping with ALL. Post-treatment, children will have regular follow-up visits with their oncology team to monitor for relapse and manage any long-term side effects. Psychological support, educational adjustments, and access to survivorship programs can help children transition back to normal life and school.
- Most children return to normal activities over time.
- Effective long-term monitoring and healthy lifestyle choices support ongoing wellness.
Frequently Asked Questions (FAQs)
Q: What is the difference between acute and chronic leukemia?
A: Acute leukemia, such as ALL, develops rapidly and requires urgent treatment, while chronic leukemia progresses slowly and may not need immediate intervention.
Q: Can ALL in children be cured?
A: Yes. Most children with ALL are cured with modern treatment protocols. The five-year survival rate exceeds 85% in many countries.
Q: What are the chances of ALL returning after treatment?
A: While relapse is possible, intensive follow-up helps detect recurrence early. Additional therapy, such as a stem cell transplant, may be considered if the disease returns.
Q: Is ALL hereditary?
A: ALL is rarely inherited. Certain genetic conditions can increase risk, but most children diagnosed do not have a family history of the disease.
Q: What support is available for families coping with a childhood leukemia diagnosis?
A: Pediatric cancer centers offer multidisciplinary support: medical care, psychological counseling, social services, educational assistance, and survivorship programs for children and their families.
Key Takeaways
- Acute lymphoblastic leukemia (ALL) is the most common childhood cancer. Early diagnosis and treatment are crucial.
- Most symptoms are due to low blood cell counts (anemia, bleeding, infection risk).
- The majority of children with ALL are cured after multi-phase chemotherapy and supportive care.
- Regular follow-up helps manage both short- and long-term effects of therapy.
References
- https://www.chop.edu/conditions-diseases/acute-lymphoblastic-leukemia-all
- https://www.mayoclinic.org/diseases-conditions/acute-lymphocytic-leukemia/symptoms-causes/syc-20369077
- https://kidshealth.org/en/parents/all.html
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5520400/
- https://www.stjude.org/care-treatment/treatment/childhood-cancer/leukemia-lymphoma/acute-lymphoblastic-leukemia-all.html
- https://www.uwhealth.org/conditions/pediatric-acute-lymphoblastic-leukemia-all
Read full bio of Sneha Tete












