Acute Lymphoblastic Leukemia (ALL) Diagnosis: Tests, Stages, and What to Expect
Learn about the step-by-step process of diagnosing acute lymphoblastic leukemia, from symptoms and screenings to specialized tests and staging.
Diagnosing Acute Lymphoblastic Leukemia (ALL): An In-Depth Guide
Acute lymphoblastic leukemia (ALL) is a type of cancer that affects the blood and bone marrow, progressing rapidly and requiring swift diagnosis and treatment. Understanding the steps and methods used for diagnosis is crucial for patients, families, and caregivers. This comprehensive article explores how ALL is diagnosed, the key tests involved, what to expect during evaluation, and why precise diagnosis matters for treatment planning.
Why Is an Accurate Diagnosis of ALL Important?
Accurately diagnosing ALL is essential because it guides treatment choices, provides critical information about the cancer’s severity, and helps predict potential outcomes. Since the symptoms of leukemia can resemble those of other diseases, thorough testing prevents misdiagnosis and ensures prompt, targeted care for the patient.
- Determines subtype: ALL has several subtypes; identifying the exact form is necessary for optimal treatment.
- Assesses spread and severity: The stage and progression of ALL impact treatment options significantly.
- Prepares for personalized medicine: Genetic and molecular tests help tailor therapies that may improve outcomes.
Recognizing Symptoms and When to Seek Medical Advice
Symptoms of ALL can be subtle at first, often mimicking infections or other benign conditions. However, persistence or escalation of symptoms warrants immediate medical attention. Common signs include:
- Persistent fatigue or weakness
- Frequent fever or infections
- Unexplained bruising or bleeding
- Pale skin
- Bone or joint pain
- Swollen lymph nodes, liver, or spleen
- Unexplained weight loss
- Night sweats
- Shortness of breath or dizziness
These symptoms arise due to the overproduction of immature white blood cells that crowd out healthy blood cells in the bone marrow. While these signs do not confirm ALL, they are a vital reason to consult a healthcare provider for further investigation.
Initial Evaluation: Medical History and Physical Examination
The journey toward an ALL diagnosis often begins with a thorough review of medical history and a physical exam. The healthcare provider will ask about the onset and duration of symptoms, any personal or family history of cancer, previous illnesses, and exposure to risk factors.
- Physical exam checks for:
- Swollen lymph nodes in the neck, armpits, or groin
- Enlarged liver or spleen (palpable in the abdomen)
- Unusual skin findings such as bruises or rashes
- Signs of infection or inflammation
While a physical exam cannot confirm leukemia, it provides essential clues that direct subsequent testing and helps to rule out other causes of the symptoms.
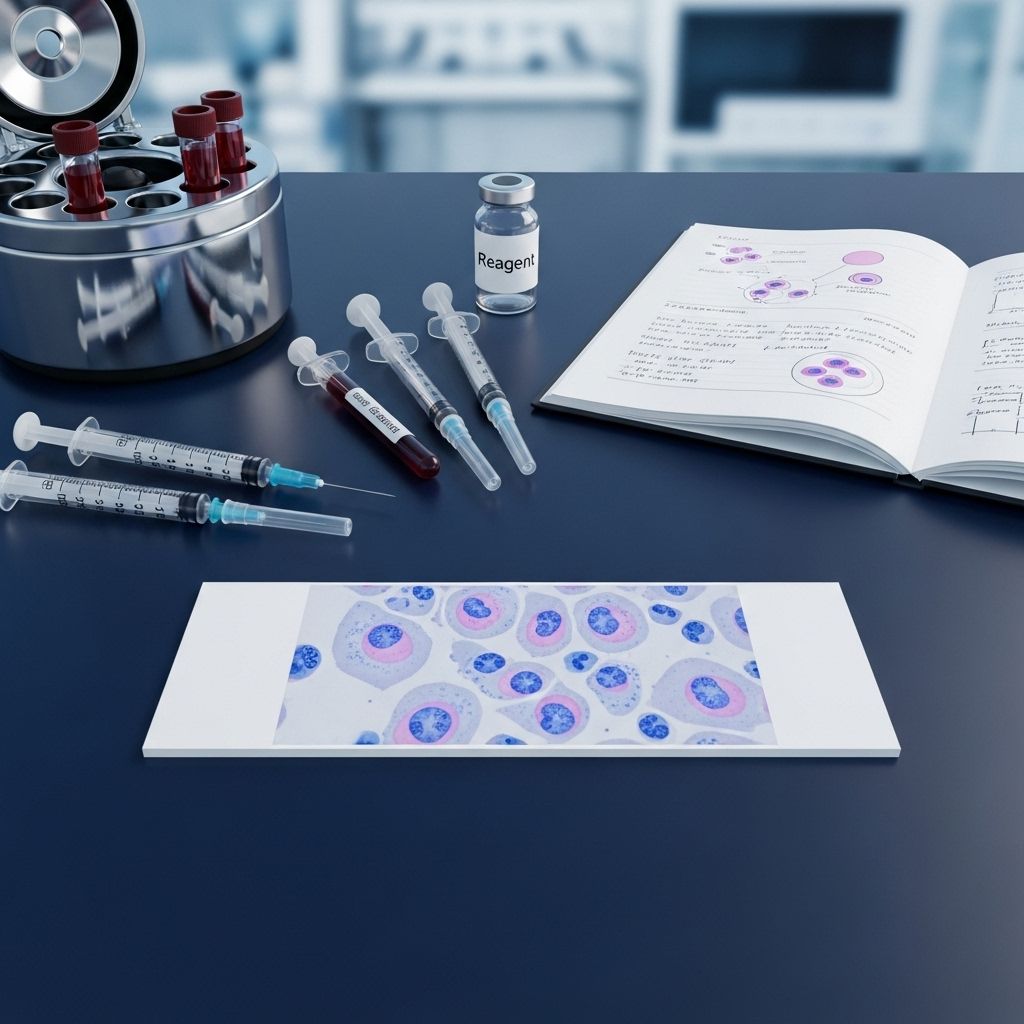
Blood Tests: The Key to ALL Diagnosis
Blood tests are the backbone of leukemia diagnosis. They reveal significant abnormalities that often prompt further tests. The most common blood investigations include:
- Complete Blood Count (CBC): Measures the number and appearance of red blood cells (RBCs), white blood cells (WBCs), and platelets.
- Peripheral Blood Smear: Examines the shape and maturity of blood cells under a microscope, focusing on abnormal or immature cells (blasts).
- Comprehensive Metabolic Panel: Assesses organ function and detects complications.
- Coagulation Tests: Evaluates clotting functions that may be impaired in leukemia.
A CBC is often the first test ordered due to its ability to detect leukemia’s classic hallmarks: elevated WBCs, low platelets, and low RBCs. The peripheral blood smear provides visual confirmation of abnormal or immature cell types.
What Blood Test Results Might Indicate ALL?
If leukemia is present, a CBC and peripheral blood smear may reveal:
- High or very low white blood cell count
- High numbers of immature white blood cells (blasts)
- Low platelet and red blood cell counts
- Abnormal appearance of blood cells
These findings are suggestive but not definitive. Confirmatory tests follow abnormal blood results.
Bone Marrow Tests: Confirming the Diagnosis
The gold standard for confirming ALL is a bone marrow aspiration and biopsy. This procedure detects and analyzes leukemia cells directly at their source.
- Bone marrow aspiration: A liquid sample is withdrawn from inside the bone (often the hip bone) using a thin, hollow needle and local anesthesia.
- Bone marrow biopsy: Often performed at the same time, this procedure uses a thicker needle to remove a small core of bone marrow tissue for examination.
Lab analysis of bone marrow samples confirms the presence, proportion, and specific type of leukemia cells. Special staining, flow cytometry, and molecular testing pinpoint the exact ALL subtype and can identify critical markers such as chromosomal changes or gene mutations.
Possible Experiences During Bone Marrow Collection
- The area is numbed with a local anesthetic to minimize pain.
- Some pressure or brief sharp pain may be felt during aspiration or biopsy.
- Most people can return home shortly after the procedure.
- Mild soreness or bruising at the site is common and temporary.
Additional Diagnostic Tests: Imaging and Spinal Fluid Analysis
After blood and bone marrow analysis, further testing may be ordered to:
- Assess the spread of leukemia
- Detect organ involvement or complications
- Stage the leukemia for prognosis and treatment planning
Imaging Studies
- Chest X-ray: Can show lymph node or organ enlargement
- Ultrasound: Useful for assessing liver, spleen, and kidney size
- CT (Computed Tomography) Scan: Provides detailed cross-sectional images of internal organs
- MRI (Magnetic Resonance Imaging) Scan: Helps evaluate brain, spinal cord, and other soft tissue involvement
- PET (Positron Emission Tomography) Scan: Detects areas of active cancer in the body
Lumbar Puncture (Spinal Tap)
A lumbar puncture is used to test whether leukemia cells are present in the cerebrospinal fluid (CSF) that surrounds the brain and spinal cord:
- The procedure involves inserting a thin needle between the bones of the lower spine to withdraw a small sample of CSF.
- A local anesthetic is used to reduce discomfort.
- The fluid is analyzed for leukemia cells and infection.
This test is particularly important because some forms of ALL can spread to the central nervous system, and treatment may need to be adjusted accordingly.
Specialized Laboratory Analyses
Advanced testing techniques assist in classifying ALL and evaluating prognosis:
- Flow cytometry: Examines the proteins on cell surfaces to determine the type and maturity of leukemia cells.
- Cytogenetic analysis: Detects chromosomal abnormalities, such as translocations or deletions, which affect prognosis and treatment decisions.
- Molecular testing: Looks for gene mutations (e.g., Philadelphia chromosome) that can influence therapy.
- Immunophenotyping: Identifies distinct cellular markers using antibodies, further clarifying ALL subtype.
Staging and Risk Assessment in ALL
Unlike solid tumors, ALL is not staged in the traditional sense based on size or spread. Instead, staging focuses on how the cancer affects blood and marrow and whether it has invaded the central nervous system or organs. Key staging factors include:
- Initial WBC count at diagnosis
- Age at diagnosis
- Subtypes of ALL identified through genetic or molecular testing
- Response to initial treatment (remission status)
- Evidence of leukemia in CSF (central nervous system involvement)
Doctors use these factors, along with specialized scoring systems, to assign a risk category (standard, intermediate, high), which guides the intensity and type of therapy.
How Doctors Monitor and Assess ALL During and After Treatment
- Periodic blood counts: Track remission status and detect recurrence.
- Minimal residual disease (MRD) testing: Uses molecular or flow cytometric techniques to detect small numbers of residual leukemia cells after treatment.
- Repeat bone marrow exams: Confirm remission or detect early relapse.
- Liver and kidney function tests: Monitor organ health during therapy.
- Imaging and lumbar puncture (as needed): Evaluate for signs of spread or complications.
Comprehensive, repeated evaluations allow for early intervention if ALL does not respond to initial treatment or relapses later.
Table: Key Diagnostic Tests for ALL and Their Purposes
| Test | Purpose |
|---|---|
| Physical Exam & Medical History | Initial assessment for signs and risk factors |
| Complete Blood Count (CBC) | Measures blood cell counts and detects abnormalities |
| Peripheral Blood Smear | Examines blood cell maturity/appearance |
| Bone Marrow Aspiration/Biopsy | Confirms diagnosis, identifies subtype |
| Flow Cytometry/Immunophenotyping | Classifies leukemia cells, guides treatment |
| Cytogenetics/Molecular Testing | Finds genetic changes, affects prognosis/treatment choice |
| Imaging (CT, MRI, X-ray, PET) | Assesses organ involvement or spread |
| Lumbar Puncture | Detects leukemia in the cerebrospinal fluid |
Frequently Asked Questions (FAQs)
Q: What is the first step in diagnosing ALL?
A: The first step is usually a review of symptoms and medical history, followed by a physical exam. Abnormal findings prompt blood tests such as a CBC and blood smear.
Q: Can leukemia be diagnosed with a blood test alone?
A: Blood tests may strongly suggest leukemia, but a bone marrow aspiration or biopsy is required to definitively diagnose ALL and determine its type.
Q: Why are so many tests needed to diagnose ALL?
A: Multiple tests are necessary to confirm the presence of leukemia, define its specific characteristics, rule out other diseases, and guide treatment decisions based on risk factors and cancer subtype.
Q: What does staging mean in ALL?
A: For ALL, staging involves assessing how far the leukemia has affected the blood, bone marrow, other organs, and the central nervous system. This process guides therapy by assigning a risk category rather than a numerical stage.
Q: How quickly is an ALL diagnosis made after symptoms appear?
A: A preliminary diagnosis can usually be made within a few days after symptoms prompt initial blood work. Full classification and staging, including genetic testing, may take several days to weeks.
What to Expect: Preparing for Diagnosis and Next Steps
Facing an acute lymphoblastic leukemia diagnosis can be overwhelming. Most diagnostic procedures are outpatient, require minimal preparation, and use local anesthetics or sedation as needed. Supportive care teams and counseling services are available to guide patients and families through the process. The results of these investigations will shape the overall treatment plan, which is usually started promptly after a confirmed diagnosis.
- Expect rapid communication between doctors, pathologists, and specialists.
- Bring a support person to appointments when possible.
- Ask questions and seek out information—understanding the process can help reduce anxiety and empower decision-making.
Summary
Diagnosing acute lymphoblastic leukemia is a multi-step process that integrates symptoms, physical findings, blood tests, bone marrow evaluation, genetic analysis, and imaging. Each step provides crucial information, moving from suspicion to a confirmed diagnosis and helping craft a personalized treatment strategy. Staying informed can make this challenging period more manageable and foster active participation in care decisions.
References
- https://www.healthline.com/health/leukemia
- https://www.webmd.com/cancer/lymphoma/understanding-leukemia-basics
- https://www.nursetogether.com/leukemia-nursing-diagnosis-care-plan/
- https://www.healthline.com/health/leukemia/leukemia-diagnosis
- https://www.medicalnewstoday.com/articles/321692
- https://www.medicalnewstoday.com/articles/142595
- https://www.patientpower.info/leukemia/leukemia-diagnosis
- https://www.healthline.com/health/video/cll-community-stories-2
- https://my.clevelandclinic.org/health/diseases/4365-leukemia
- https://www.healthline.com/health/video/cll-information-and-stories
Read full bio of Sneha Tete












