Acute Coronary Syndrome vs. Coronary Artery Disease: Key Differences and Connections
Understanding acute coronary syndrome and coronary artery disease, their relationship, risk factors, symptoms, and treatments for a healthier heart.
Acute Coronary Syndrome vs. Coronary Artery Disease: Understanding the Connection
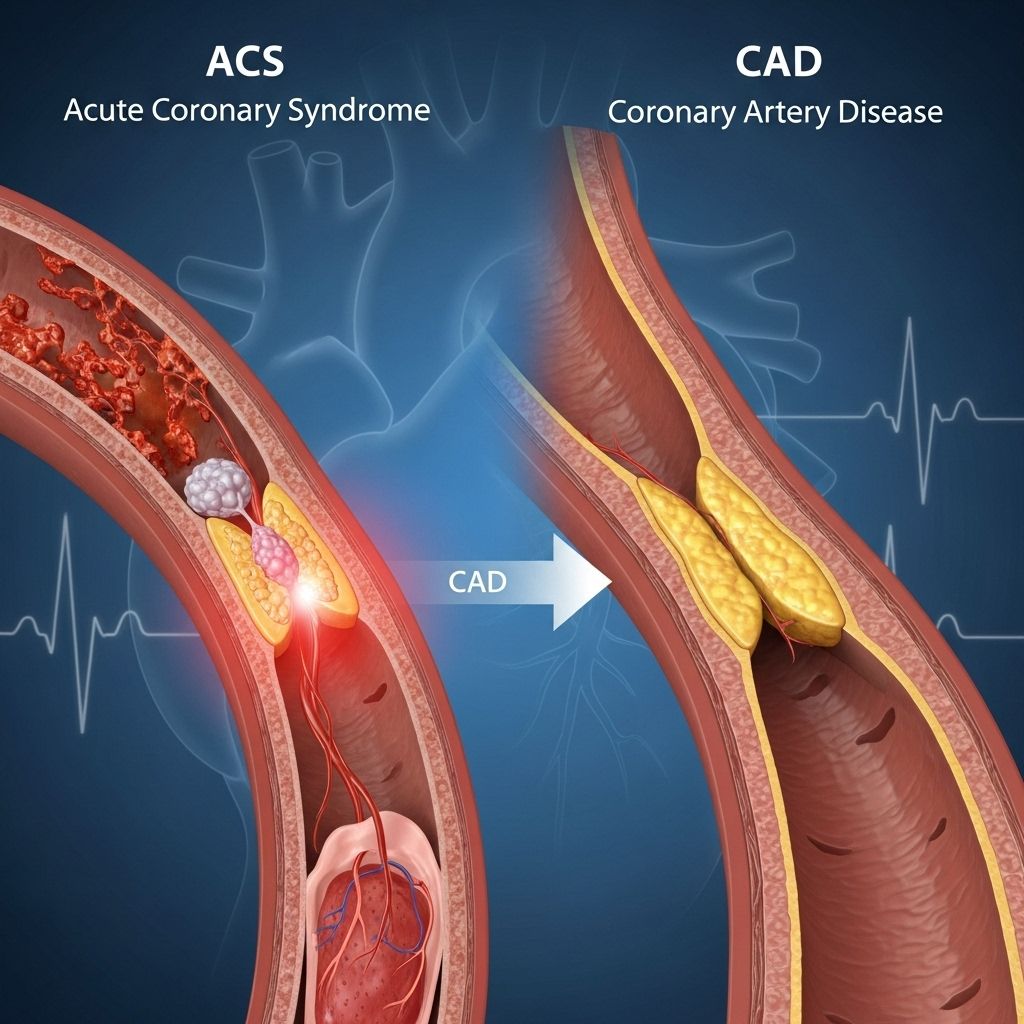
Acute coronary syndrome (ACS) and coronary artery disease (CAD) are closely related, often causing confusion due to their overlapping symptoms and shared origins. However, these are distinct cardiac conditions, each with unique implications for risk, emergency response, and long-term heart health management. This article offers an in-depth comparison, outlines their individual features, and explains how they are linked by common causes and risk factors.
What Is Coronary Artery Disease (CAD)?
Coronary artery disease (CAD) is a chronic condition characterized by the progressive narrowing or blockage of the arteries supplying blood to the heart muscle. As the most common type of heart disease, CAD affects millions worldwide and is a leading cause of morbidity and mortality.
- CAD primarily develops due to atherosclerosis, a buildup of plaque comprised of cholesterol, fatty deposits, calcium, and other substances within the coronary arteries.
- This plaque buildup narrows the lumen (the blood-carrying channel), leading to reduced myocardial (heart muscle) blood supply, a process that may go unnoticed for years.
- As arteries become stiffer and less responsive to bodily demands, blood flow may become insufficient, especially during activities that increase the heart’s workload.
- In advanced stages, plaque can rupture, triggering the formation of a blood clot (thrombus) and potentially leading to a heart attack.
CAD often remains silent—producing little to no symptoms until it significantly impairs blood flow or causes a related complication such as angina or myocardial infarction.
Key Features of CAD
- Chronic, slow-progressing disease
- Caused by gradual plaque buildup (atherosclerosis)
- Symptoms often limited in early stages, may include chest pain (angina), shortness of breath, or fatigue
- Major risk factor for heart attack and other acute cardiac events
What Is Acute Coronary Syndrome (ACS)?
Acute coronary syndrome (ACS) is a medical emergency referring to a cluster of conditions directly precipitated by a sudden reduction or complete blockage of blood flow to part of the heart. Unlike the more gradual development of CAD, ACS arises abruptly and requires urgent attention.
- ACS always presents with symptoms—most commonly chest pain—marking an acute event in the heart’s blood supply.
- It occurs as a result of pre-existing CAD, specifically when an unstable plaque ruptures or erodes, causing blood clots and sharply reducing or blocking blood flow.
Types of ACS
ACS is an umbrella term describing three related, but clinically distinct, cardiac events:
- Unstable angina: Characterized by sudden or unpredictable chest pain, often occurring at rest and representing a significant warning sign. Unlike stable angina, which is triggered by exertion and relieved by rest, unstable angina may persist or worsen and is considered a precursor to a heart attack.
- Non-ST-elevation myocardial infarction (NSTEMI): A type of heart attack identified by specific blood markers indicating heart muscle damage, but without the classic changes seen on an electrocardiogram (ECG). NSTEMI typically results from a partial or brief blockage in a coronary artery.
- ST-elevation myocardial infarction (STEMI): A more severe form of heart attack. STEMI is diagnosed by dramatic ECG changes (ST-segment elevation) and high levels of cardiac enzymes in the blood. It is caused by a prolonged, complete blockage that damages a significant part of the heart muscle.
Comparing CAD and ACS
| Coronary Artery Disease (CAD) | Acute Coronary Syndrome (ACS) | |
|---|---|---|
| Nature | Chronic and progressive | Acute, sudden onset |
| Main Feature | Plaque buildup, artery narrowing | Sudden blockage due to plaque rupture |
| Symptoms | Often asymptomatic; may experience stable angina | Always symptomatic: unstable angina, heart attack |
| Diagnosis | Imaging, stress tests, blood lipids | ECG, blood tests for heart enzymes, clinical presentation |
| Urgency | Manageable, with lifestyle and medication | Medical emergency; immediate intervention necessary |
Causes and Risk Factors for CAD and ACS
CAD and ACS are fundamentally linked by their underlying cause—atherosclerosis—and they share many risk factors, though ACS typically arises from an acute complication of long-standing CAD.
Primary Causes
- Plaque buildup (atherosclerosis): Gradual accumulation of cholesterol, fat, and inflammatory cells in the wall of the coronary arteries
- Plaque rupture: In ACS, an unstable atherosclerotic plaque breaks open, prompting a blood clot to form and abruptly obstructing the artery
Risk Factors for Both CAD and ACS
- High blood pressure (hypertension)
- High cholesterol
- Cigarette smoking
- Diabetes
- Obesity or being overweight
- Physical inactivity
- Unhealthy diet (high in saturated/trans fats, low in fruits/vegetables)
- Genetic predisposition/family history of heart disease
- Older age
- Chronic stress
Although the risk factors are similar for both conditions, it is the instability of a plaque—and the body’s reaction to its rupture—that transforms stable CAD into the acute emergency of ACS.
Treatment Approaches
Both CAD and ACS require immediate and sometimes long-term treatment strategies, but the urgency and focus of each approach differs significantly.
Treating CAD
- Lifestyle modifications: Including dietary changes, smoking cessation, increased physical activity, and weight management
- Medications:
- Statins to reduce cholesterol
- Antihypertensives to manage blood pressure
- Antiplatelet agents to prevent clot formation
- Beta blockers and nitrates for angina control
- Procedures: In severe cases, doctors may recommend coronary angioplasty (stent placement) or coronary artery bypass grafting (CABG) to restore or improve blood flow.
Treating ACS
- Emergency interventions:
- Immediate administration of oxygen, aspirin, nitroglycerin, and pain relief (such as morphine)
- Anti-clotting medications (thrombolytics or anticoagulants)
- Urgent percutaneous coronary intervention (PCI), commonly known as angioplasty with possible stent insertion
- Coronary artery bypass surgery in select cases
- Post-ACS management: Lifelong heart-protective measures, including all aspects of CAD management, cardiac rehabilitation, and close medical supervision
Who Is Most at Risk for ACS?
- People with existing CAD: Those with advanced or poorly managed coronary artery disease have the highest risk, as their plaque buildup may rupture suddenly.
- Men and post-menopausal women: Men are typically at higher risk at younger ages; risk increases for women after menopause due to declining estrogen levels.
- History of heart attack or stroke: Previous cardiovascular events increase the likelihood of plaque instability and further acute episodes.
- Individuals with multiple cardiovascular risk factors: Especially smokers, diabetics, people with uncontrolled hypertension, or those with a strong family history of heart disease.
Symptoms: Recognizing CAD and ACS
Common Symptoms of CAD
- Angina (chest pain or discomfort, usually triggered by exertion)
- Shortness of breath during activity
- Fatigue
- Palpitations
Symptoms of Acute Coronary Syndrome
- Sudden onset chest pain or pressure (often radiating to the arm, neck, or jaw)
- Chest pain at rest (unstable angina)
- Shortness of breath
- Nausea or vomiting
- Profuse sweating
- Dizziness or fainting
- Anxiety, unusual fatigue, or sense of impending doom
If ACS is suspected, immediate emergency medical care is essential to limit heart muscle damage and improve outcomes.
Preventing CAD and ACS
- Follow a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins
- Engage in regular physical activity (at least 150 minutes per week of moderate-intensity exercise)
- Maintain a healthy weight and avoid tobacco products
- Manage chronic conditions such as high blood pressure, diabetes, and high cholesterol effectively
- Reduce stress through mindfulness, relaxation, or counseling as needed
Frequently Asked Questions (FAQs)
What is the most important difference between CAD and ACS?
CAD is a chronic, progressive narrowing of the coronary arteries due to plaque buildup, while ACS describes the sudden, symptomatic, and potentially life-threatening events (like heart attacks and unstable angina) that occur when a plaque ruptures or becomes unstable and suddenly impairs or blocks blood flow.
Can you have CAD without ACS?
Yes. Many people live for years with CAD that is managed or stable and never progress to ACS, especially with proactive risk factor management and medical care.
Are the risk factors for CAD and ACS the same?
They are fundamentally the same—high blood pressure, high cholesterol, smoking, diabetes, obesity, inactivity, and family history—but ACS represents an abrupt complication of existing CAD.
How are CAD and ACS diagnosed?
- CAD: Non-invasive imaging, coronary angiography, stress tests, ECG, and blood lipid analysis.
- ACS: Emergency ECG assessment, blood tests for heart enzymes (troponin), chest pain characteristics, and possibly angiogram.
What should you do if you suspect ACS?
Call emergency medical services immediately. Prompt treatment is critical to prevent permanent heart muscle damage or death.
Takeaway
Acute coronary syndrome and coronary artery disease are interconnected cardiovascular conditions. CAD sets the stage over years, and ACS signals an urgent, severe complication—often a heart attack—that can be life-threatening. Early diagnosis, diligent risk management, and lifestyle changes can help prevent or limit the progression of both, improving survival and long-term quality of life.
References
- https://www.healthline.com/health/heart-health/acute-coronary-syndrome-vs-coronary-artery-disease
- https://atlanticcardiovascular.com/blog/cad-vs-acs/
- https://my.clevelandclinic.org/health/diseases/22910-acute-coronary-syndrome
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4958723/
- https://www.youtube.com/watch?v=Xihun54Gqhw
- https://www.siloamhospitals.com/en/informasi-siloam/artikel/coronary-artery-disease-vs-acute-coronary-syndrome
- https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.117.028991
Read full bio of medha deb












