Acute Coronary Syndrome: Symptoms, Causes, Diagnosis, and Treatment
Understand acute coronary syndrome—its warning signs, causes, diagnosis steps, and effective treatment strategies for heart health.
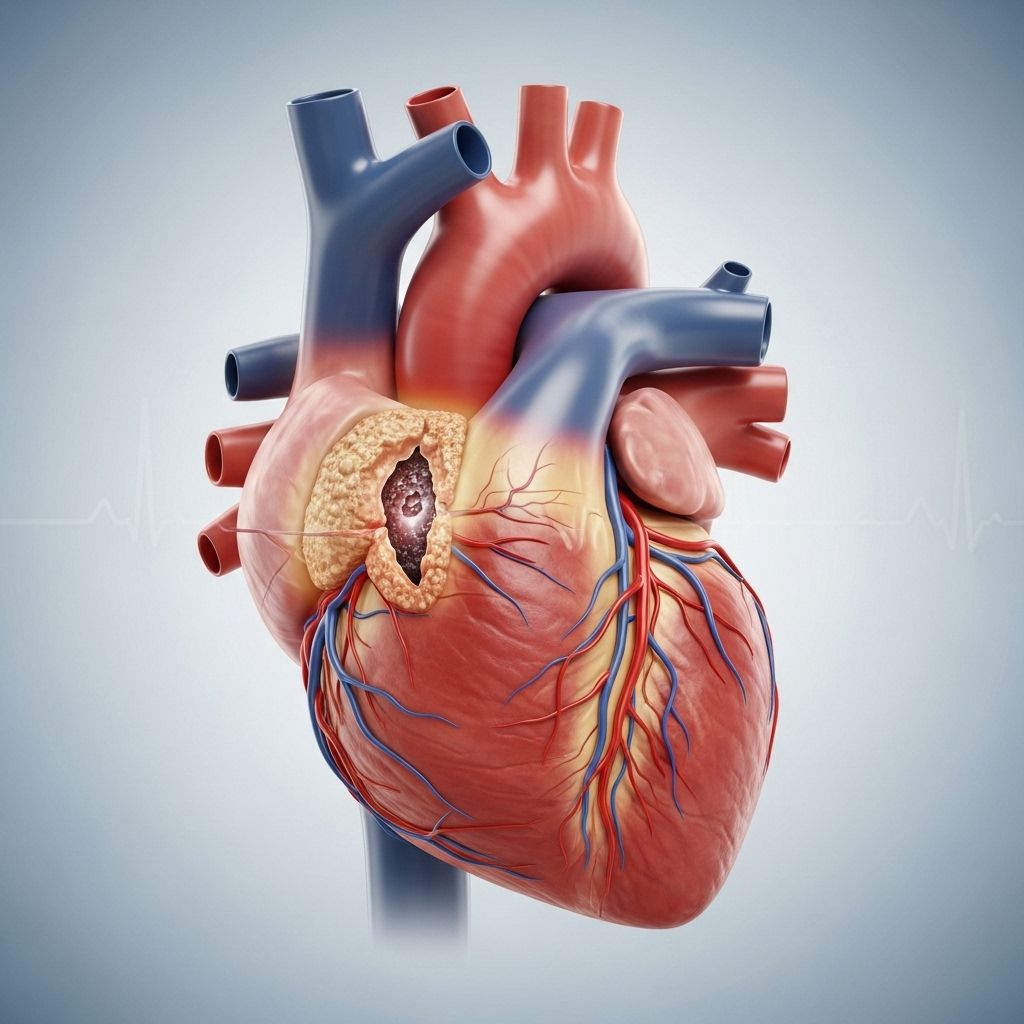
Acute coronary syndrome (ACS) refers to a set of clinical conditions associated with a sudden, significant reduction in blood flow to the heart muscle. This interruption is most commonly caused by blockage of the coronary arteries and can be life-threatening if not promptly treated. ACS can result in heart attack (myocardial infarction) or unstable angina. Immediate medical attention is essential to restore blood flow, minimize heart muscle damage, and improve survival rates.
What Is Acute Coronary Syndrome?
Acute coronary syndrome is an umbrella term used for a range of conditions that occur due to reduced blood flow in the coronary arteries, the vessels that supply the heart muscle with oxygen-rich blood. It includes:
- Unstable angina: New or worsening chest pain/pressure that may occur at rest or with minimal exertion and does not resolve easily.
- Non-ST-elevation myocardial infarction (NSTEMI): A less severe type of heart attack where there is partial blockage or damage, confirmed by blood tests showing heart muscle injury.
- ST-elevation myocardial infarction (STEMI): A severe heart attack caused by total blockage, visible on an electrocardiogram (ECG).
ACS is a medical emergency, as the oxygen supply to the heart muscle is compromised, which can lead to permanent tissue damage or death if not treated quickly.
Symptoms of Acute Coronary Syndrome
The symptoms of ACS often develop rapidly and may be severe. Recognizing the signs early and seeking immediate care can be lifesaving. Typical symptoms include:
- Chest pain or discomfort: This is the most frequent symptom, often described as pressure, tightness, fullness, squeezing, or an aching sensation in the center or left side of the chest. It may come on suddenly, come and go, or worsen over time.
- Pain extended to other areas: Discomfort may radiate to the shoulders, arms (especially the left arm), back, neck, jaw, or stomach.
- Shortness of breath: Difficulty breathing can accompany or follow chest pain.
- Sweating: Profuse, cold sweat is common with ACS.
- Nausea or vomiting: Stomach upset or actual vomiting may develop.
- Lightheadedness or dizziness: Fainting or feeling like you may pass out.
- Rapid or irregular heartbeat: Unusually fast (tachycardia), pounding, or irregular heartbeat (palpitations).
- Fatigue: Unusual tiredness, sometimes days before other symptoms in women or elderly people.
- Anxiety: Feeling impending doom or panic without apparent cause.
Symptoms may vary by age, gender, and presence of other health conditions. Women, older adults, and people with diabetes may have atypical symptoms, such as unexplained fatigue, discomfort in other areas (like the jaw or back), or shortness of breath without chest pain.
Causes of Acute Coronary Syndrome
The immediate cause of ACS is a sudden reduction or complete halt in the blood flow through a coronary artery. This is usually the result of:
- Plaque rupture: Fatty plaques made of cholesterol, fat, calcium, and other substances build up inside artery walls. If a plaque ruptures, a blood clot may form at the site, suddenly narrowing or fully blocking the artery.
- Blood clot (thrombus) formation: The body’s response to plaque rupture often causes a blood clot, which can partially or completely obstruct the coronary artery.
- Severe arterial narrowing: Over time, arteries can become so narrowed from plaque buildup that reduced blood flow triggers ACS symptoms, even if a clot has not formed.
Less commonly, ACS can be caused by:
- Sudden tightening or spasm of the coronary artery
- Dissection (a tear in the artery wall)
- In rare instances, severe infections or other serious medical conditions
Risk Factors
Certain risk factors increase the likelihood of developing acute coronary syndrome:
| Non-Modifiable | Modifiable |
|---|---|
| Age (men ≥ 45, women ≥ 55) | High blood pressure (hypertension) |
| Family history of heart disease | High cholesterol levels |
| Genetics | Diabetes |
| Obesity (BMI ≥ 30) | |
| Physical inactivity | |
| Cigarette smoking or drug abuse | |
| Excessive alcohol consumption | |
| High stress levels |
When to Seek Immediate Help
Acute coronary syndrome is a medical emergency. Call 911 immediately if you or someone else experiences sudden chest pain or discomfort, especially when accompanied by shortness of breath, sweating, nausea, vomiting, palpitations, or fainting. Quick action can save lives and limit heart damage.
Diagnosis of Acute Coronary Syndrome
Rapid and accurate diagnosis of ACS is crucial for effective treatment. The evaluation typically includes:
- Medical history and physical examination: The doctor will assess symptoms, risk factors, and family history.
- Electrocardiogram (ECG or EKG): Measures the electrical activity of the heart and detects changes suggesting a heart attack or unstable angina.
- Blood tests:
- Cardiac enzymes (troponin levels): Elevated levels indicate damage to the heart muscle.
- Other markers: To rule out other conditions.
- Imaging tests:
- Chest X-ray: Checks for other causes of symptoms.
- Echocardiogram: Ultrasound to visualize heart structure and function.
- Coronary angiography: Injection of dye into heart vessels followed by X-ray to locate blockages.
- Stress testing (after stabilization): Assesses how the heart functions under exertion or medication-induced stress.
Treatment of Acute Coronary Syndrome
The main goals of ACS treatment are to restore blood flow, relieve symptoms, protect the heart muscle from further damage, and prevent future complications. Treatment approaches include immediate interventions, medications, lifestyle changes, and sometimes surgical procedures.
Initial Emergency Care
- Administration of oxygen (if needed)
- Pain relief: Nitroglycerin under the tongue to widen arteries and relieve chest pain
- Aspirin or other antiplatelet drugs to prevent further clotting
- Continuous monitoring of vital signs and heart rhythm
Medications
- Clot busters (Thrombolytics): Help dissolve clots that are blocking arteries. Most effective when given early.
- Antiplatelet agents: Medications such as aspirin, clopidogrel, or prasugrel prevent new blood clots from forming.
- Beta blockers: Help the heart muscle relax, slow heart rate, lower blood pressure, and reduce heart workload.
- ACE inhibitors: Relax blood vessels, improve blood flow, and lower blood pressure.
- Angiotensin II receptor blockers (ARBs): Used as alternatives to ACE inhibitors for blood pressure and vessel relaxation.
- Calcium channel blockers: Relax and open blood vessels and can lower heart rate.
- Statins: Lower cholesterol levels and stabilize plaque in arteries to prevent rupture.
- Other cholesterol-lowering medicines: Such as ezetimibe, which limit cholesterol absorption.
- Alpha blockers and central agonists: Occasionally used to control blood pressure in select cases.
Procedures and Surgery
- Angioplasty and stenting: A catheter with a balloon is used to open blocked arteries; a stent (small mesh tube) is often placed to keep the artery open.
- Coronary artery bypass grafting (CABG): Surgery to create a new route around blocked arteries using blood vessel grafts from elsewhere in the body.
Lifestyle Changes for Ongoing Heart Health
- Quit smoking: The single most effective action to reduce future heart attack risk.
- Heart-healthy diet: Focus on fruits, vegetables, lean proteins, whole grains, and minimal saturated fat.
- Regular physical activity: Under doctor guidance, aim for most days of the week.
- Weight management: Achieving and maintaining a healthy weight lessens stress on the heart.
- Manage coexisting conditions: Control blood pressure, cholesterol, and blood sugar (if diabetic).
- Limit or avoid alcohol: Excessive alcohol increases heart risk.
- Stress management: Practice techniques such as mindfulness, meditation, or counseling.
- Routine medical follow-up: Keep ongoing appointments for check-ups and medication adjustment.
Prevention Strategies
While not all risk factors can be controlled, the following steps greatly reduce the risk of developing ACS or experiencing another event:
- Control high blood pressure and cholesterol through diet, exercise, and medications as needed
- Maintain a healthy body weight
- Adopt a physically active lifestyle
- Avoid tobacco use—seek medical help if needed to quit
- Limit alcohol intake, if consumed at all
- Effectively manage diabetes and other chronic conditions
- Find constructive ways to handle stress
Outlook and Recovery
With prompt treatment, many people recover well from acute coronary syndrome. The degree of recovery depends on:
- The extent of heart damage
- How quickly treatment began after symptoms started
- The presence and control of other health conditions
Cardiac rehabilitation, a medically supervised program of exercise and education, is highly recommended after ACS events to help patients improve heart health, adopt healthy habits, and safely return to daily activities.
Frequently Asked Questions (FAQs)
Q: What is the main difference between unstable angina and heart attack?
A: Both are forms of acute coronary syndrome involving reduced blood flow to the heart. In a heart attack (myocardial infarction), the blockage is severe enough to cause heart muscle damage, observable by elevated cardiac enzymes in blood tests. Unstable angina causes symptoms but does not result in detectable heart muscle injury.
Q: Do women have the same symptoms of ACS as men?
A: While chest pain remains the most common symptom for both, women are more likely to experience additional signs such as unexplained fatigue, shortness of breath, back or jaw pain, and nausea.
Q: How quickly should I get to a hospital if I suspect ACS?
A: Immediate medical attention is crucial. Call 911 right away. Do not try to drive yourself, as the condition can rapidly worsen.
Q: Can ACS be prevented?
A: You can reduce your risk by quitting smoking, controlling high blood pressure and cholesterol, eating a heart-healthy diet, maintaining an active lifestyle, and managing stress.
Q: Will I need lifelong medication after an ACS event?
A: Most people require long-term medications, such as antiplatelets, statins, beta blockers, and possibly blood pressure medicines, to protect the heart and prevent future problems. Your doctor will tailor your treatment plan.
Q: Is cardiac rehabilitation necessary?
A: Strongly recommended after an ACS event, as rehabilitation improves recovery, reduces risk of further heart issues, and helps rebuild confidence and physical strength.
References
- https://www.mayoclinic.org/diseases-conditions/acute-coronary-syndrome/diagnosis-treatment/drc-20352140
- https://www.rwjbh.org/treatment-care/heart-and-vascular-care/diseases-conditions/acute-coronary-syndrome/
- https://www.mountsinai.org/health-library/diseases-conditions/acute-coronary-syndrome
- https://my.clevelandclinic.org/health/diseases/22910-acute-coronary-syndrome
- https://www.mayoclinic.org/diseases-conditions/acute-coronary-syndrome/symptoms-causes/syc-20352136
- https://www.ncbi.nlm.nih.gov/books/NBK459157/
- https://www.medstarhealth.org/services/acute-coronary-syndrome
- https://www.urmc.rochester.edu/conditions-and-treatments/acute-coronary-syndrome
- https://www.aafp.org/pubs/afp/issues/2017/0215/p232.html
Read full bio of medha deb












