Understanding ACE2: Its Critical Role in Type 1 Diabetes
A comprehensive exploration of how ACE2 impacts glucose regulation, pancreatic function, and complications in type 1 diabetes.
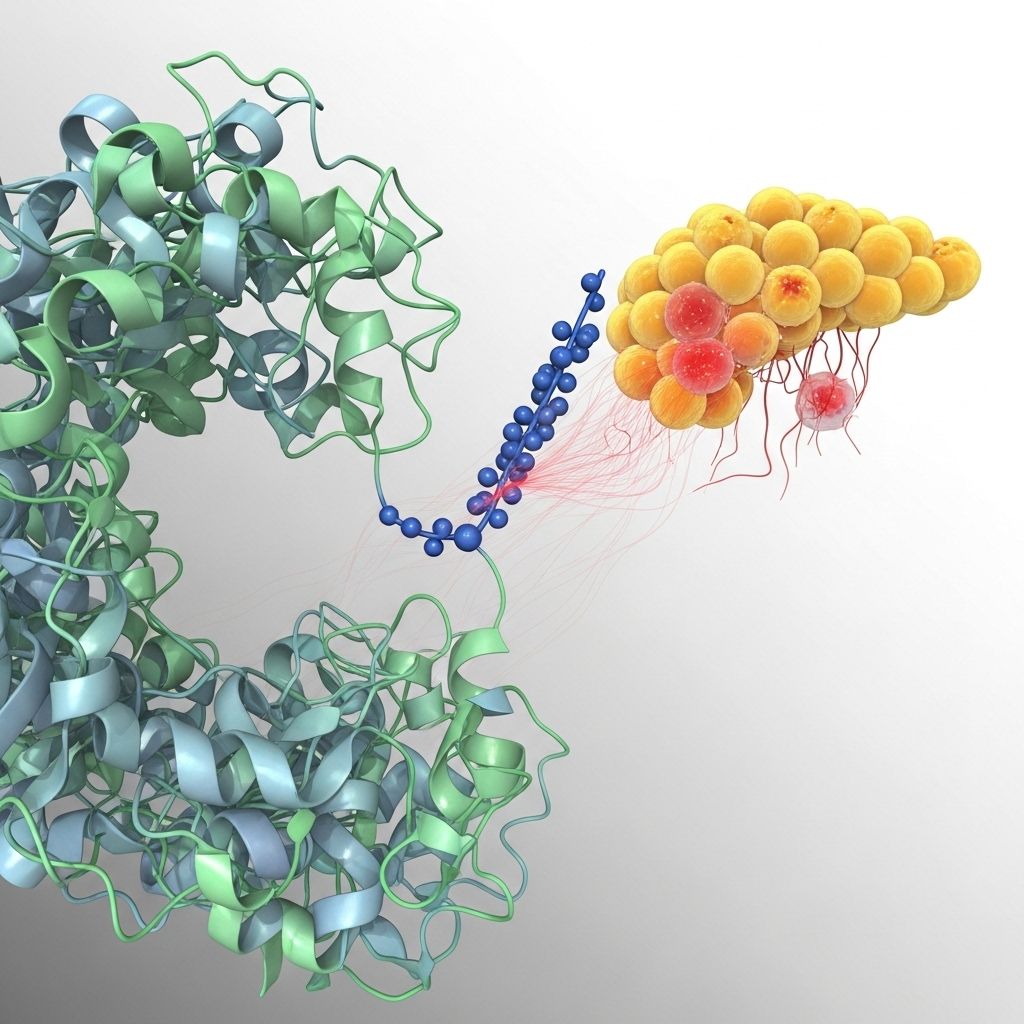
The link between angiotensin-converting enzyme 2 (ACE2) and type 1 diabetes has garnered significant attention, not only because of its importance in glucose and insulin regulation but also due to its far-reaching effects on diabetes complications and potential avenues for therapy. This in-depth article reviews the biological functions of ACE2, its connections to the pancreas and kidney, the implications for type 1 diabetes, and what the latest science suggests for the future.
What is ACE2?
ACE2 (angiotensin-converting enzyme 2) is an enzyme found throughout the body, especially in the pancreas, lungs, heart, kidneys, and gastrointestinal tract. It plays a crucial role in the renin-angiotensin system (RAS), which helps regulate blood pressure, fluid balance, and systemic vascular resistance.
- ACE2 converts angiotensin II, a peptide that can increase blood pressure and inflammation, into angiotensin-(1-7), which counters many of these effects.
- Unlike ACE (angiotensin-converting enzyme), which promotes vasoconstriction and sodium retention, ACE2 generally exerts protective, anti-inflammatory, and vasodilatory effects.
- Recent research connects ACE2 to glucose metabolism, pancreatic function, and the progression of diabetes and its complications.
How ACE2 Functions in the Body
ACE2 acts as a balance to the effects of ACE within the RAS:
- ACE converts angiotensin I to angiotensin II, leading to vasoconstriction, elevated blood pressure, and pro-inflammatory actions.
- ACE2 degrades angiotensin II to angiotensin-(1-7), producing vasodilation and anti-inflammatory responses. This enzyme’s function helps to maintain vascular and metabolic health.
In multiple tissues, including the pancreas, the balance between ACE and ACE2 determines local blood flow, inflammation, and cellular function.
ACE2 and Type 1 Diabetes: The Scientific Connection
Type 1 diabetes is a condition marked by autoimmune destruction of insulin-producing beta cells in the pancreas. This leads to fluctuations in blood glucose levels and insufficient insulin secretion. Researchers have found that ACE2:
- Is highly expressed in pancreatic islets, including beta cells, where insulin is secreted.
- Appears to support normal insulin secretion and maintain beta cell viability.
- When ACE2 is deficient or downregulated in animal models, glucose tolerance worsens and insulin secretion decreases.
The Role of ACE2 in Pancreatic Function
Within the pancreas:
- ACE2 breaks down angiotensin II, helping prevent harmful local effects such as blood flow reduction and inflammation in the islets of Langerhans (the clusters of beta and other insulin-related cells).
- Blockade of the broader RAS system (with ACE inhibitors or angiotensin II receptor blockers) has been shown in animal studies to increase pancreatic blood flow, reduce islet inflammation and fibrosis, and restore insulin production in diabetic models.
This suggests that ACE2 acts as a defender against pancreatic dysfunction, possibly slowing the progression of diabetes and its complications.
The Renin-Angiotensin System and Its Dual Nature
The renin-angiotensin system (RAS) is a hormone system regulating blood pressure, fluid balance, and vascular tone. The RAS has a “bad” and a “good” side:
- Classical RAS (ACE/Angiotensin II axis): promotes inflammation, vasoconstriction, and fibrosis — factors contributing to high blood pressure, insulin resistance, and vascular damage.
- Protective RAS (ACE2/Angiotensin-(1-7) axis): counters inflammation, promotes vasodilation, and reduces oxidative stress — essential for healthy organs, including the heart, kidney, and pancreas.
In diabetes, imbalances in this system (less ACE2, more angiotensin II) can accelerate disease progression and multi-organ damage.
How ACE2 Affects Insulin and Glucose Regulation
Insulin is the hormone critical for lowering blood glucose. Research shows the following impacts for ACE2:
- ACE2 deficiency in animal models leads to impaired first-phase insulin secretion — an early, rapid insulin release needed for proper glucose disposal.
- Blockade of RAS (either ACE or angiotensin II receptors) improves islet function, enhances insulin release, and reduces fibrosis and inflammation in the pancreas.
- ACE2 overexpression experimentally improves pancreatic beta cell function and glucose tolerance.
- Angiotensin II (the product of ACE but substrate for ACE2) can delay insulin secretion and limit islet blood flow, compounding blood sugar issues.
Thus, higher ACE2 activity may protect against the early loss of beta cell function and support insulin regulation in type 1 diabetes.
Impact of ACE2 in Diabetic Complications
Diabetes complications often develop over time and involve site-specific damage to organs:
- Kidney (diabetic nephropathy): ACE2 prevents local angiotensin II buildup, reducing proteinuria and fibrosis. ACE2 deficiency fosters glomerular injury.
- Heart and blood vessels: ACE2’s protective effects may limit cardiac dysfunction, vascular inflammation, and hypertension, which are more common in diabetes.
- Eye (diabetic retinopathy): Maintenance of gut ACE2 (not just systemic ACE2) preserves gut barrier and immune regulation, reducing inflammation and the risk/severity of diabetic retinopathy in animal models.
Table: ACE2 Effects on Organs in Type 1 Diabetes
| Organ | Effect of ACE2 Deficiency | Potential ACE2 Protection |
|---|---|---|
| Pancreas | Impaired insulin secretion, islet dysfunction | Beta cell support, better glucose tolerance |
| Kidney | Proteinuria, glomerular damage | Reduced fibrosis, less protein loss |
| Heart/Blood Vessels | Higher risk of hypertension, dysfunction | Improved cardiac and vascular health |
| Eye | Accelerated retinopathy risk | Protection against blood vessel damage in retina |
| Gut | Loss of barrier, increased inflammation | Maintained integrity, reduced inflammation |
Why Understanding ACE2 Matters for People With Type 1 Diabetes
The involvement of ACE2 in so many organs and its effects on glucose metabolism make it a compelling topic for both basic science and clinical strategy. Key reasons it matters include:
- ACE2 activity could be a future target for therapies aiming to preserve beta cells or slow down the development of complications.
- People with diabetes and high blood pressure may benefit from medications (like ACE inhibitors or angiotensin receptor blockers) that change RAS activity.
- COVID-19 research has focused on ACE2 because the virus uses it as a receptor; nevertheless, its positive role in metabolic and organ health remains crucial for understanding both risks and new treatments for people with diabetes.
Therapeutic Implications and Future Research
Although much of the current evidence on ACE2 and type 1 diabetes comes from animal models and laboratory studies, the findings carry important implications:
- RAS blockade therapies (ACE inhibitors, ARBs) have shown benefits in animal models, leading to improved insulin secretion, islet protection, and reduced kidney damage. Some clinical studies point to reduced type 2 diabetes incidence, though the data are mixed and ongoing research is needed.
- Direct ACE2 modulation (such as gene therapy or recombinant ACE2) is being explored to support pancreatic and kidney health, but is not yet available for clinical use.
- Probiotic strategies that increase intestinal ACE2 have been shown to offer protection against gut and eye complications in diabetic mice, pointing to novel future approaches.
What’s Next?
Future therapies may include:
- New drugs designed specifically to enhance ACE2 expression or activity.
- Personalized approaches, taking into account each patient’s ACE/ACE2 status and risk of complications.
- More robust human studies to clarify how ACE2-targeted treatments can both delay progression and reduce the risk of complications in type 1 diabetes.
Frequently Asked Questions (FAQs)
What is ACE2, and why is it important for type 1 diabetes?
ACE2 is an enzyme that balances the renin-angiotensin system, supporting healthy blood flow and helping to regulate glucose and insulin secretion—functions that are critical in type 1 diabetes management.
Does ACE2 deficiency cause diabetes?
Current evidence suggests that ACE2 deficiency may contribute to poor insulin secretion and possibly worsen glucose tolerance, increasing susceptibility to complications, but it is not the sole cause of diabetes.
Can medications targeting ACE2 help manage diabetes or its complications?
Medications that block the effects of angiotensin II (via ACE inhibitors or ARBs) support pancreatic and kidney health in diabetic animal studies. However, specific ACE2-targeted therapies are still in preclinical or early clinical research stages.
Is ACE2 impacted by COVID-19 in people with type 1 diabetes?
COVID-19 enters cells via ACE2 receptors, but the complex role of ACE2 in organ health means research is ongoing. Having diabetes does not necessarily mean you have more ACE2; clinical implications are not fully understood.
Are there lifestyle measures to increase ACE2 activity?
No specific lifestyle intervention is proven to increase ACE2 directly, but maintaining blood glucose control, a heart-healthy diet, and regular physical activity supports overall metabolic health and may indirectly help balance the renin-angiotensin system.
Takeaway and Action Points
- ACE2 is a critical enzyme for metabolic balance, organ protection, and regulating glucose and insulin in the context of type 1 diabetes.
- Disruption in the ACE/ACE2 axis can foster pancreatic damage, insulin deficiency, and multi-organ complications.
- Current and future research may lead to medicines that directly enhance ACE2’s beneficial effects for people with type 1 diabetes.
- Effective diabetes management and regular checkups remain essential while more ACE2-targeted treatments are being explored.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2992757/
- https://portlandpress.com/clinsci/article/126/7/471/69184/Role-of-angiotensin-converting-enzyme-2-ACE2-in
- https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.122.322003
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8646749/
- https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.772865/full
- https://www.uab.edu/news/research-innovation/type-1-diabetes-maintaining-the-enzyme-ace2-in-the-gut-prevents-diabetic-blindness
Read full bio of medha deb












