ACE Inhibitors: How They Support Heart and Kidney Health
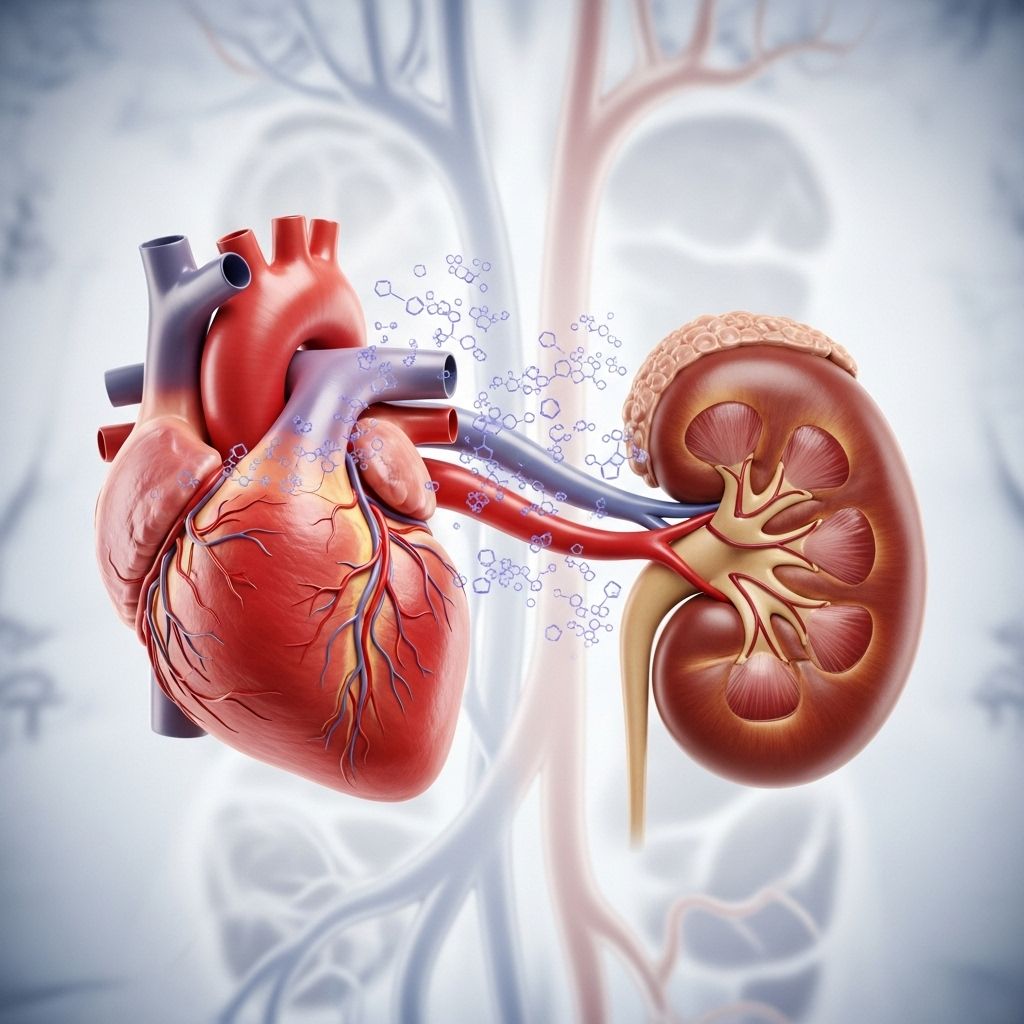
ACE inhibitors play a key role in treating heart failure, hypertension, and kidney conditions by relaxing blood vessels and easing cardiac workload.
Angiotensin-converting enzyme inhibitors—commonly known as ACE inhibitors—are a cornerstone in the treatment of conditions like high blood pressure, heart failure, and certain kidney disorders. Their impact on cardiovascular and renal health has made them a first-line therapy for millions worldwide. This guide explains how ACE inhibitors work, their uses, potential side effects, and what patients can expect.
What Are ACE Inhibitors?
ACE inhibitors are a class of prescription medications used predominantly to treat hypertension (high blood pressure), heart failure, and various kidney disorders. These drugs target the angiotensin-converting enzyme in the body, decreasing the production of a hormone that constricts blood vessels. By relaxing and widening blood vessels, ACE inhibitors make it easier for the heart to pump blood and help lower blood pressure, ultimately reducing cardiovascular strain and boosting kidney function.
How Do ACE Inhibitors Work?
The mechanism of ACE inhibitors revolves around the renin-angiotensin-aldosterone system (RAAS), which regulates blood pressure and fluid balance. Here’s a simplified breakdown:
- The kidneys release an enzyme called renin into the bloodstream when blood pressure drops or sodium levels are low.
- Renin converts angiotensinogen (from the liver) into angiotensin I.
- The angiotensin-converting enzyme (ACE) transforms angiotensin I into angiotensin II—a powerful vasoconstrictor that narrows blood vessels and stimulates the release of hormones that raise blood pressure.
- ACE inhibitors block this conversion, resulting in less angiotensin II, so blood vessels relax and widen. This lowers blood pressure and reduces the volume of fluid the heart must pump.
This makes ACE inhibitors an effective option for reducing the workload on the heart and improving circulation throughout the body, especially to vital organs such as the heart and kidneys.
Common Conditions Treated with ACE Inhibitors
ACE inhibitors are prescribed for several conditions, either alone or alongside other medications. Major uses include:
- High Blood Pressure (Hypertension): ACE inhibitors are recommended to lower elevated blood pressure, helping prevent heart attacks, strokes, and kidney problems.
- Heart Failure: They are first-line drugs to support heart function, reduce symptoms such as breathlessness and swelling, and improve survival rates.
- Post-Heart Attack (Myocardial Infarction): These drugs can be started after a heart attack, especially in people with reduced heart pumping capacity, to protect and strengthen the heart muscle.
- Chronic Kidney Disease (CKD): ACE inhibitors help slow the progression of kidney disease, particularly in diabetes or when protein is present in urine.
- Other Uses: ACE inhibitors may also be used to manage conditions like proteinuria (protein in urine), glomerular diseases of the kidney, and to prevent further damage following kidney transplantation.
Examples of ACE Inhibitor Medications
Several ACE inhibitors are approved and widely prescribed. While they work via a similar mechanism, they differ in duration of action and dosage. Notable examples include:
- Lisinopril (Zestril, Prinivil)
- Enalapril/Enalaprilat (Vasotec)
- Ramipril (Altace)
- Captopril (Capoten)
- Benazepril (Lotensin)
- Fosinopril (Monopril)
- Quinapril (Accupril)
- Moexipril (Univasc)
- Perindopril (Aceon)
- Trandolapril (Mavik)
The main difference between these medications is how long their effects last (short-acting vs. long-acting), which can determine how often they need to be taken each day.
How Are ACE Inhibitors Used?
ACE inhibitors are typically administered as tablets or capsules, taken once or twice daily depending on the specific drug and condition being treated. Doctors will determine the starting dose and carefully adjust it according to your response and any side effects. It’s important to take the medication around the same time every day and never stop without first consulting your doctor.
| ACE Inhibitor | Brand Names | Typical Frequency |
|---|---|---|
| Lisinopril | Zestril, Prinivil | Once daily |
| Enalapril | Vasotec | Once or twice daily |
| Ramipril | Altace | Once or twice daily |
| Captopril | Capoten | Two or three times daily |
| Benazepril | Lotensin | Once or twice daily |
Who Should Take ACE Inhibitors?
ACE inhibitors are often the first choice for individuals with:
- High blood pressure, particularly if they also have diabetes, heart failure, or kidney disease
- Heart failure, to reduce symptoms and boost survival
- Recent heart attack, especially with left ventricular dysfunction or heart failure
- Chronic kidney disease, especially with proteinuria
They may be used alone or in combination with other blood pressure medications. Physicians may recommend ACE inhibitors even to people who have no symptoms but carry risk factors like diabetes, high cholesterol, or a family history of heart disease.
Benefits of ACE Inhibitors
Research demonstrates several significant benefits for patients taking ACE inhibitors:
- Reduced blood pressure, lowering the risk of strokes and heart attacks
- Improved heart function, especially in heart failure
- Decreased progression of chronic kidney disease, particularly in diabetic patients
- Lower risk of cardiovascular events and mortality in at-risk individuals
- Protection of the heart following a heart attack and slowing of heart muscle remodeling, helping to avoid future complications
Potential Side Effects of ACE Inhibitors
Most people tolerate ACE inhibitors well, but some side effects are possible. The most common include:
- Dry, persistent cough – a well-known side effect that may lead some patients to switch medications
- Increased blood potassium levels (hyperkalemia), potentially dangerous if severe
- Low blood pressure (hypotension), especially after the first dose or when dehydrated
- Fatigue and dizziness, particularly when starting therapy or with dose increases
- Headache
- Changes in kidney function, requiring periodic blood tests
- Rare: Allergic reactions or swelling (angioedema), usually at the lips, tongue, or throat
Tell your healthcare provider if you experience bothersome or severe side effects. In some cases, switching to another class of medications, such as angiotensin receptor blockers (ARBs), might resolve persistent issues like cough.
Precautions and Interactions
ACE inhibitors should not be used during pregnancy, as they can cause harm to an unborn baby. Caution is also warranted in people with:
- History of angioedema
- High potassium levels
- Severe kidney disease or bilateral renal artery stenosis
Concurrent use with other medications—such as potassium-sparing diuretics, certain painkillers (NSAIDs), and some supplements—can increase the risk of side effects or reduce effectiveness. Always inform your doctor of all medicines and supplements you are taking.
Monitoring and Regular Checks
When starting ACE inhibitor therapy, doctors will typically:
- Order initial and periodic blood tests to check kidney function and potassium levels
- Monitor blood pressure regularly, especially in the first weeks of treatment or after dose changes
- Instruct you to report any signs of swelling, rash, muscle weakness, chest pain, or severe dizziness
These precautions help ensure that ACE inhibitors are both safe and effective for your long-term treatment plan.
Frequently Asked Questions (FAQs)
What do ACE inhibitors do in simple terms?
They relax blood vessels and help the heart pump more efficiently by inhibiting the production of a hormone that usually tightens your blood vessels. This action lowers blood pressure and supports heart and kidney health.
How long do ACE inhibitors take to work?
Most people see their blood pressure drop within several hours or days. Maximum effects for heart or kidney benefits typically require ongoing, daily use.
Can ACE inhibitors be taken long-term?
Yes, they are designed for long-term use to prevent health complications. Periodic monitoring by a healthcare professional is needed.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s nearly time for your next dose. Never double up. Consistency is important for best results.
What are alternatives to ACE inhibitors?
Alternatives include angiotensin II receptor blockers (ARBs), calcium channel blockers, diuretics, and beta-blockers. Your doctor will choose based on your medical history, condition, and response to treatment.
Key Takeaways: ACE Inhibitors
- ACE inhibitors are widely used to control blood pressure, treat heart failure, and help protect kidney health.
- They work by blocking the conversion of angiotensin I to angiotensin II, resulting in relaxed blood vessels and reduced strain on the heart.
- Common side effects include cough, elevated potassium, and low blood pressure—most are mild and manageable.
- Regular monitoring and communication with your healthcare provider maximize their benefits and minimize risk.
- Never stop or adjust your dose without medical advice—sudden changes can be dangerous.
When to Seek Emergency Help
- Sudden swelling of lips, tongue, face, or throat (possible angioedema)
- Severe dizziness or fainting
- Chest pain or signs of an allergic reaction
Call emergency services if you have any of these symptoms after starting an ACE inhibitor.
Summary
ACE inhibitors are a foundational therapy for managing high blood pressure, heart failure, and kidney disease. Their effectiveness at relaxing blood vessels, protecting the heart, and preserving kidney function make them a go-to medication for many chronic health concerns. By understanding how these drugs work and staying closely monitored by your healthcare team, you can maximize benefits while minimizing any risks.
References
- https://www.ncbi.nlm.nih.gov/books/NBK430896/
- https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/drug-cabinet/ace-inhibitors
- https://www.ncbi.nlm.nih.gov/books/NBK431051/
- https://www.medicalnewstoday.com/articles/ace-inhibitors-for-heart-disease
- https://www.youtube.com/watch?v=xIlaQuRaZmk
- https://my.clevelandclinic.org/health/treatments/21934-ace-inhibitors
- https://www.webmd.com/heart-disease/guide/medicine-ace-inhibitors
- https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.120.16667
Read full bio of Sneha Tete












