6 Subtle Warning Signs of a Heart Attack a Month Before
Recognize often-overlooked symptoms that may indicate a heart attack is approaching, and learn how to take action.
Heart attacks are often perceived as sudden, dramatic events, but mounting scientific evidence and patient experiences show that early, often subtle symptoms may occur weeks before a major cardiovascular event. Recognizing these warning signs—and acting before the heart attack actually happens—can be life-saving. This article explores the six common signs that may appear up to a month prior to a heart attack, examines why they occur, how to interpret them, and when to seek medical care.
Table of Contents
- Overview: How Heart Attacks Develop
- 6 Early Warning Signs
- Heart Attack Risk Factors
- What to Do If You Notice Symptoms
- Prevention Tips
- Frequently Asked Questions
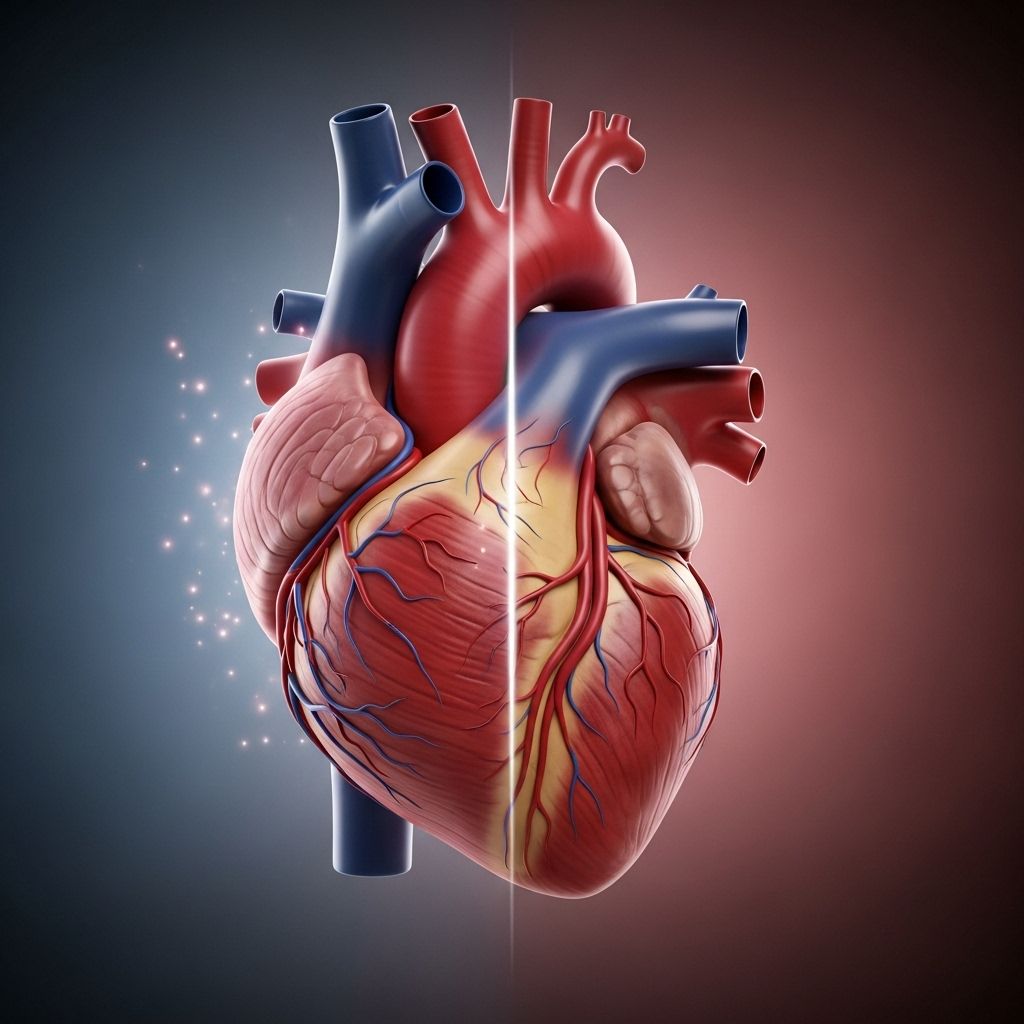
How Do Heart Attacks Develop?
A heart attack (myocardial infarction) occurs when blood flow to part of the heart is blocked, often due to a buildup of plaque in the coronary arteries—sometimes followed by rupture and formation of a blood clot. Without enough oxygen-rich blood, heart muscle cells begin to die, causing severe, sometimes irreversible damage. While heart attacks can be sudden, many people report symptoms that develop and intensify over days or weeks. These early signs are your body’s cry for help and should never be ignored.
The 6 Warning Signs You May Notice a Month Before a Heart Attack
Not all symptoms are dramatic. Research and clinical experience suggest you may encounter a cluster of subtle signs, sometimes mistaken for other issues. Here’s what to watch for:
1. Unusual Fatigue
Feeling inexplicably wiped out or experiencing persistent fatigue is a common yet often overlooked warning. Up to 70% of heart attack survivors report having felt unusually tired in the days or weeks before their event. Unlike normal fatigue, this symptom:
- Lingers for days, regardless of rest
- May make simple tasks exhausting
- Is unrelated to increased physical or mental workload
- Frequently affects women more than men
Fatigue may result from the heart’s reduced ability to circulate oxygen-rich blood efficiently throughout the body, or from inflammation and hormonal shifts linked to heart disease.
2. Disrupted or Poor Sleep
Trouble sleeping, including insomnia, frequent waking, or restless nights, can coincide with heart disease. While poor sleep can have many causes, recent studies link it to heart attack risk, especially when paired with other symptoms. You might notice:
- Difficulty staying asleep
- Unusual restlessness or tossing and turning
- Waking up gasping for air (possible sign of heart failure)
Chronic poor sleep can be a sign that your heart isn’t functioning optimally or that fluid is starting to build up around lungs (pulmonary edema). Poor sleep increases physiological stress, further taxing the heart.
3. Shortness of Breath
Struggling to catch your breath or feeling winded after minimal activity can point to underlying cardiovascular trouble. This symptom may:
- Occur even at rest or during light exertion
- Be accompanied by chest discomfort
- Indicate fluid accumulation in the lungs (sign of failing heart)
Shortness of breath results when the heart cannot efficiently pump blood, leading to a backup of fluid in the lungs and a reduction in oxygen supply.
4. Digestive Issues or Abdominal Discomfort
Symptoms such as indigestion, heartburn, nausea or abdominal pain can precede a heart attack. These are often mistaken for mild gastroenterological problems, but when persistent (especially in individuals with risk factors), they should be evaluated carefully.
- Persistent indigestion with or without chest discomfort
- Nausea or vomiting not explained by food or illness
- Sense of fullness or bloating even after small meals
Women are more likely than men to experience these digestive-related symptoms during heart attacks.
5. Unexplained Chest Discomfort
The most classic warning sign, chest pain or discomfort can be subtle and intermittent, presenting as:
- Pressure, squeezing, fullness, or pain in the center or left side of the chest
- Pain that lasts more than a few minutes or comes and goes
- Mild aching, tightness, or burning sensation
The discomfort may radiate to the arms (often the left), back, neck or jaw. Some people describe it as “an elephant sitting on my chest”.
6. Pain or Discomfort in Other Areas
Pre-heart attack symptoms can also include pain or discomfort in non-chest areas:
- Arms, especially the left (but can affect both)
- Shoulders
- Neck
- Jaw
- Upper back
This pain often builds gradually and may wax and wane. It is caused by “referred pain,” where nerve signals spread from the heart to nearby areas of the body.
| Symptom | Typical Features |
|---|---|
| Fatigue | Persistent, unexplained, worsens over days |
| Sleep disturbances | Insomnia, frequent waking, restless nights |
| Shortness of breath | Occurs with minimal activity or rest |
| Digestive issues | Indigestion, nausea, abdominal pain |
| Chest discomfort | Subtle pressure, tightness, fullness, pain |
| Pain in other areas | Arms, jaw, back, neck, shoulders |
Who Is at Risk: Understanding Heart Attack Risk Factors
Several conditions and lifestyle factors can increase your risk of heart attack and the likelihood of experiencing early warning signs. These include:
- Advanced age—risk increases with age
- Family history of heart disease
- High blood pressure
- High cholesterol, especially LDL
- Obesity
- Poor diet (high in saturated fats, low in fruits/vegetables)
- Excess alcohol consumption
- Smoking
- Physical inactivity
- Chronic stress
- Diabetes
Your risk also varies based on gender. Women may experience less typical symptoms (such as nausea, fatigue, anxiety, and shoulder pain), while men more often report classic chest pain.
What Should You Do If You Notice Early Warning Signs?
If you recognize one or more of these warning signs—especially if you’re at higher risk—don’t ignore them or wait for them to resolve. Immediate steps include:
- Call emergency services (911 or local number) if symptoms are severe, sudden, or worsening
- Describe your symptoms clearly to medical personnel
- Stay calm and follow professional instructions
- If symptoms are mild but persistent, book a medical evaluation within days
- Track when symptoms began and how often they occur
- Avoid driving yourself to the hospital if chest pain is present
Timely intervention—from medication to diagnostic tests—can prevent or reduce long-term damage.
Prevention: How to Lower Your Risk of a Heart Attack
The most effective strategies to prevent heart attacks involve lifestyle changes and proactive health management. Key tips include:
- Control blood pressure, cholesterol, and diabetes with regular monitoring and therapy
- Eat a heart-healthy diet rich in vegetables, whole grains, lean protein, and healthy fats
- Stay physically active—aim for at least 150 minutes of moderate exercise weekly
- Maintain a healthy weight
- Avoid smoking and limit alcohol intake
- Manage stress through mindfulness, coping skills, and counseling if needed
- Take medications as prescribed for any cardiac or metabolic condition
- Get regular health checkups—even if you feel fine
Recognizing subtle symptoms early, especially with a focus on prevention, can save lives. Sharing information with loved ones and creating an action plan improves the chances of surviving an event.
Frequently Asked Questions (FAQs)
Q: Can symptoms like fatigue or indigestion really be signs of a heart attack?
A: Yes. Though these symptoms are common and have many causes, persistent, unusual fatigue or digestive issues in people with risk factors may signal decreased heart function and warrant further evaluation.
Q: Do women experience different heart attack symptoms?
A: Women tend to have more non-classic symptoms, such as nausea, vomiting, fatigue, shoulder and jaw pain, and may not always have chest pain. These signs can be less dramatic but are no less serious.
Q: How long before a heart attack do these symptoms typically occur?
A: Warning signs can appear days to weeks before a heart attack, sometimes even a month or longer. The frequency and severity tend to build gradually, although sudden, severe symptoms warrant immediate emergency attention.
Q: Is chest pain always present with a heart attack?
A: No. Many people—especially women—may have little or no chest pain and predominantly experience other symptoms such as fatigue, shortness of breath, or pain in other areas.
Q: What should I do if I suspect I’m having a heart attack?
A: Call emergency services (911) immediately. Do not attempt to drive yourself to the ER. Early medical intervention can be the difference between life and death.
Takeaway
Heart attacks rarely strike out of the blue. Listening to your body, especially when symptoms develop quietly over weeks, is essential to prevention and survival. If you or someone you know is at risk, keep this list of warning signs in mind and act promptly.
References
- https://www.heart.org/en/health-topics/heart-attack/warning-signs-of-a-heart-attack
- https://www.healthline.com/health/heart-disease/warning-signs-heart-attack
- https://www.heartfoundation.org.au/blog/5-warning-signs-of-a-heart-attack-you-may-not-know
- https://www.medicalnewstoday.com/articles/151444
- https://www.nhs.uk/conditions/heart-attack/
- https://health.clevelandclinic.org/early-signs-of-a-heart-attack
- https://www.nhlbi.nih.gov/health/heart-attack/symptoms
- https://www.mayoclinic.org/diseases-conditions/heart-attack/symptoms-causes/syc-20373106
Read full bio of medha deb












