5 Practical Ways to Protect and Nurture Your Liver Health
Discover five actionable, evidence-based strategies to support liver function and prevent liver disease for lifelong wellness.
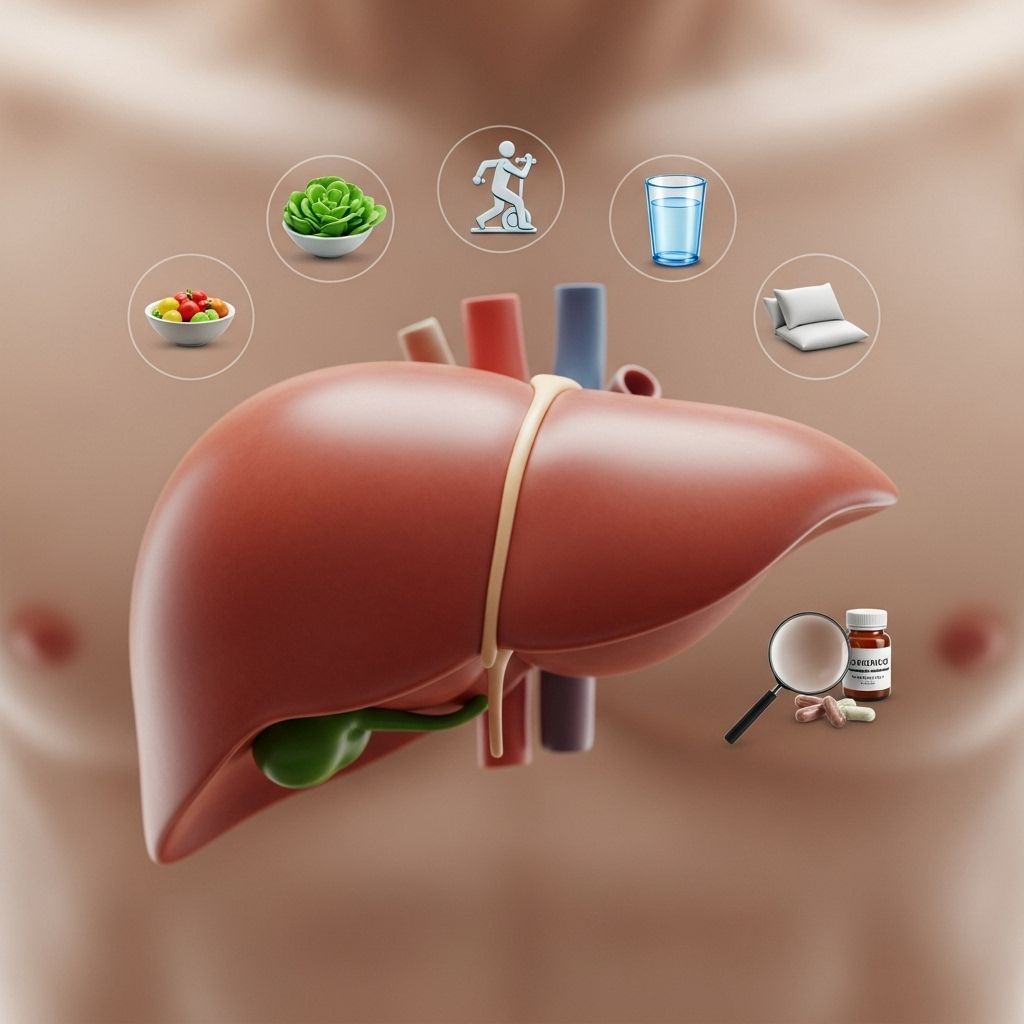
The liver is one of the most crucial organs in your body, responsible for hundreds of essential functions that range from processing nutrients, detoxifying harmful substances, to supporting metabolism and immunity. Despite its vital role and impressive ability to regenerate, the liver is susceptible to damage from lifestyle factors, environmental exposures, and genetics. Chronic liver diseases—such as fatty liver, hepatitis, cirrhosis, and liver cancer—are rising globally. The good news is that most liver disease is preventable with informed lifestyle choices. Explore these five key strategies for keeping your liver healthy and resilient throughout life.
Understanding the Liver’s Essential Role
The liver sits just below the rib cage on your right side and weighs roughly three pounds in adults. Every minute, about 1.5 quarts of blood flow through the liver, where it:
- Filters toxins, bacteria, and harmful substances from the bloodstream
- Processes nutrients from food for use by your body
- Stores vitamins, minerals, and sugars for later energy needs
- Produces bile to help digest fats
- Regulates clotting factors needed to stop bleeding
When the liver is overburdened or injured, it cannot work efficiently, leading to a cascade of health issues.
1. Eat a Well-Balanced, Nutritious Diet
What you eat directly affects your liver. Overconsumption of processed foods, trans fats, sugar, and salt can contribute to liver inflammation, fatty buildup, and ultimately impaired function. A diet rooted in whole foods supports liver health and lowers the risk of nonalcoholic fatty liver disease (NAFLD), a common cause of chronic liver problems.
- Focus on:
- Plenty of fruits and vegetables, especially leafy greens and brightly colored produce
- Whole grains like oats, brown rice, and quinoa
- Lean proteins from fish, turkey, chicken, beans, lentils, or tofu
- Healthy fats such as nuts, avocado, olive oil, and fatty fish
- Limit:
- Added sugars—found in soda, candy, and many packaged foods
- Refined carbohydrates and white flour products
- Saturated and trans fats common in fast food, processed snacks, and baked goods
- Salt, which can raise blood pressure and increase risk of edema in those with liver disease
Specific foods such as coffee (in moderation), green tea, berries, leafy greens, and cruciferous vegetables have been shown in studies to contain antioxidants and compounds that may reduce liver inflammation.
2. Exercise Moderately and Maintain a Healthy Weight
Being overweight or obese increases the risk of NAFLD, which can progress to cirrhosis or liver cancer over time. Regular physical activity not only supports weight control but also boosts metabolism and helps decrease fat accumulation around the liver.
- Aim for at least 150 minutes of moderate-intensity activity per week, such as brisk walking, cycling, or swimming.
- Add strength training exercises two days per week to preserve muscle mass and metabolic health.
- Even small amounts of regular movement can help reduce liver fat and support overall organ function.
Rapid weight loss, however, can stress the liver; talk to a healthcare provider before undertaking any diet or exercise program, especially if you have or are at risk for liver disease.
3. Minimize Alcohol Consumption
Alcohol is a leading cause of preventable liver damage worldwide. The liver metabolizes alcohol, but excessive or chronic consumption overwhelms the organ, leading to steatosis (fatty liver), hepatitis, cirrhosis, and liver cancer. The risk is higher for women and those with coexisting health problems.
- For liver health, consider limiting or abstaining from alcohol.
- If you choose to drink:
- Men: no more than two standard drinks per day
- Women: no more than one standard drink per day
One standard drink equals 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of liquor.
- You can reduce your risk further by taking days off from drinking each week or choosing nonalcoholic alternatives.
For people with existing liver disease, experts recommend complete abstinence from alcohol. If you find it difficult to reduce your intake, seek help from a healthcare provider or support group.
4. Use Medications and Supplements Wisely
The liver processes not just food and drink but also prescription drugs, over-the-counter (OTC) medicines, and dietary supplements. Certain medications, when used incorrectly, can cause liver injury. Herbal products, believed ‘natural’ and safe, can also be harmful in high doses or when combined with other drugs.
- Follow medication instructions.
- Never exceed the recommended dose, especially for acetaminophen (Tylenol), nonsteroidal anti-inflammatory drugs (NSAIDs), and statins.
- Be wary of mixing alcohol with pain relievers; this significantly increases liver risks.
- Before taking herbal supplements like kava, comfrey, or high-dose green tea extract, consult a healthcare professional.
- Update your medication list regularly and inform your healthcare provider about all prescription, OTC, and herbal remedies you use.
Certain vitamins and supplements—especially in large amounts—can also stress the liver. Vitamins A, D, E, and iron are particularly risky in overdose. Always seek professional guidance about any new supplement, particularly if you have existing liver issues or other chronic conditions.
5. Protect Yourself from Hepatitis and Toxins
Viral hepatitis—hepatitis A, B, and C—are leading global causes of liver inflammation and long-term liver disease. In addition, exposure to environmental toxins, chemicals, and household cleaning agents can silently damage liver tissue.
- Get vaccinated.
- Hepatitis A and B vaccines are available and recommended for at-risk individuals.
- There is currently no vaccine for hepatitis C. Routine blood tests can screen at-risk adults for this infection.
- Practice safe behaviors.
- Use condoms to prevent sexual transmission of hepatitis B and C.
- Never share needles, razors, toothbrushes, or any items that may have blood on them.
- Be cautious with tattoos and piercings; ensure needles are sterile and practitioners are licensed.
- Minimize toxin exposure.
- Wear gloves and masks when working with pesticides, solvents, or other chemicals.
- Keep your home well-ventilated and use nontoxic cleaners whenever possible.
- Wash fruits and vegetables thoroughly to remove pesticides or contaminants.
If you work in healthcare or at-risk environments, take additional precautions to avoid needle-stick injuries and exposure to blood-borne viruses.
When to See a Healthcare Provider
Liver disease often develops silently. Symptoms may be absent, mild, or vague until advanced stages. Be alert for signs such as:
- Yellowing of skin or eyes (jaundice)
- Unexplained fatigue or weakness
- Swelling of belly, legs, or ankles
- Dark urine or pale stool
- Persistent nausea or loss of appetite
If you notice these symptoms or have risk factors such as obesity, diabetes, heavy alcohol use, or a family history of liver disease, talk to your healthcare provider about screening. Blood tests, ultrasound, and other exams can detect liver abnormalities early, when interventions are most effective.
Liver Health Myths vs. Facts
| Myth | Fact |
|---|---|
| “Only heavy drinkers get liver disease.” | NAFLD, hepatitis, medications, and genetics can damage the liver regardless of alcohol intake. |
| “Liver cleanses and detox diets support liver function.” | The liver is self-cleansing; no evidence supports special detox regimens. Focus on balanced nutrition. |
| “Once you have liver disease, nothing can help.” | Early stages of many liver diseases are reversible with lifestyle changes and medical interventions. |
| “All supplements are safe for the liver.” | Some herbal and vitamin supplements can cause severe liver damage if misused. |
Frequently Asked Questions (FAQs)
What are the early signs of liver problems?
The most common early signs include fatigue, mild abdominal discomfort, mild swelling, unexplained weight loss, and jaundice (yellowing of the skin or eyes). However, many people have no symptoms until liver function is significantly impaired.
Should I do a detox diet or cleanse for my liver?
No scientific evidence supports the use of detox diets or cleanses for liver health. The liver can naturally eliminate toxins if it is healthy. Instead, focus on nutritious foods, maintaining a healthy weight, limiting alcohol, and practicing safe behaviors.
How often should I get my liver tested?
If you have risk factors (obesity, high alcohol intake, hepatitis, diabetes, a family history of liver disease), annual screening with blood tests and/or imaging may be recommended. Otherwise, discuss liver screening with your healthcare provider during regular check-ups.
Can herbal supplements be harmful to the liver?
Yes, certain herbal products, especially those not regulated or taken in large doses, can cause liver inflammation or even failure. Examples include kava, comfrey, and high-dose green tea extracts. Always speak with a healthcare professional before starting any new supplement.
If I have liver disease, can it be reversed?
Some forms of liver damage, such as fatty liver and early-stage inflammation, are reversible if addressed early through lifestyle changes and medical treatment. Severe scarring (cirrhosis) may be permanent, but progression can be slowed with proper care.
Key Takeaways: Simple Steps for a Healthier Liver
- Adopt a plant-based, low-sugar, low-fat diet rich in vegetables, fruits, and lean protein
- Exercise regularly and aim for a healthy body weight
- Limit alcohol or stop altogether, particularly if you have risk factors
- Use medications and supplements cautiously under medical supervision
- Protect yourself from hepatitis through vaccination and safe practices
Your liver is your body’s silent workhorse. By making conscious, informed choices every day, you can greatly reduce your risk of liver disease and enjoy better health for years to come.
References
Read full bio of Sneha Tete












